Welcome back everybody!
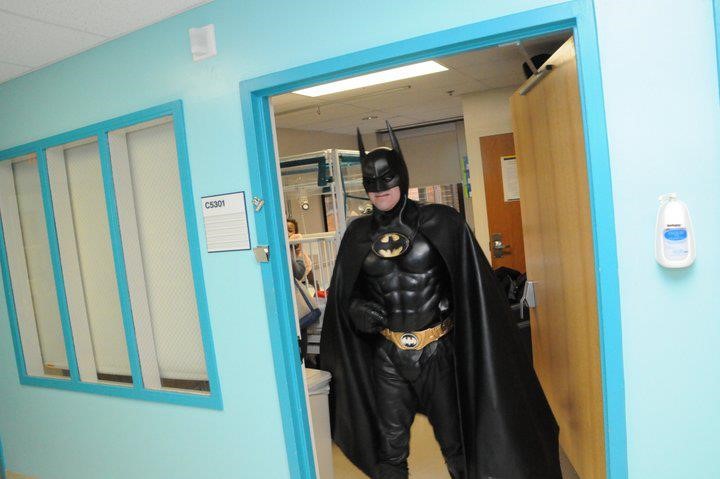
Last month, I wrote about some projects I did while rotating through the pathology program at Danbury Hospital in Connecticut. This month I’m in a more clinical setting with a hematology/oncology clerkship at Northwell’s Staten Island University Hospital. But, over the past few months of rotations (and arguably a lot longer before medical school) I’ve been noticing a part of laboratory medicine which often intersects with our clinical colleagues at the bedside. I’ve told you about the pitfalls and successes in the relationships between surgeons and anatomic pathologists before, where frozen sections are critical and time is of the essence. And we’ve all seen collaboration between the bench and bedside before—think microbiology and infectious disease, blood bank and literally everyone, etc. Still, one collaborative effort sort of happens behind the shadows, behind phone calls and lab reports, and sometimes with no communication at all! So, what kind of vigilante medicine am I talking about? Who is this Batman of medicine? It’s just our friends in hematology.
When you’re working the hematology bench in the lab, it’s pretty commonplace for a physician on a hematology service to call and ask for a peripheral smear to review. Many times, it’s for the purpose of teaching residents, fellows, or medical students but more often than not it’s a confirmatory exercise. See, when that hematologist asks to review a slide, she’s probably coming down to the lab to look at the morphology of red cells and white cells to help in their differential diagnosis. They might have a patient with a suspected thalassemia or hemoglobinopathy and, before starting the full work up of lab tests, just want to see if there are any RBC morphology traits or target cells that stand out. Thrombocytopenia? Let’s make sure there’s no platelet clumping. Maybe they’ve got a patient with some kind of liver or kidney pathology and are on the hunt for acantho- or echinocytes. Or better yet, someone went hiking, there’s an infectious etiology on their differential—let’s go hunting for babesia, malaria, oh or even erlichia!

I know what you’re thinking. Wait—that’s our job as medical laboratory scientists; our literal job. Our instruments, that we validate, and correlate, and make sure work fantastically give us flags. We investigate those flags and look at smears ourselves! We collaborate with other lab techs, and with our pathologist colleagues and send out final lab results with all kinds of helpful information: including platelet clumping, microorganisms, RBC and WBC morphology, and loads more. What gives?
Hold on to your lab coats. I’ll get there in a minute.
Slide review and differential training in medical school and residency
[This section intentionally left blank]

A Differential, Differential
So let me address the issue I brought up: why do hematologists come down to the lab to look at the slides themselves, when perfectly capable BOC certified, degree-holding medical laboratory scientists and pathologists sign out validated differentials? It might not happen this way at all hospitals, but I think the answer is a simple two-part problem.
First, as with the many things I’ve learned in medical school, one of the lab-centric pieces of information that is well understood is that, well, no one really knows what the lab does and how it operates. Virtually nobody knows the depth and breadth of the testing that pathologists manage, let alone the scientific precision and accuracy that instrument validation requires. Learning that MLS techs are certified, can hold graduate degrees, and even do their own research is often surprising to most of our clinical colleagues. And—I will tell you for a fact—that pathology and laboratory testing methodology is not covered in medical school the way you might think. Pathology is more of a class of distinguishing the identifying details of a disease, not understanding the interdisciplinary diagnostic teamwork that goes into those CBC index results on a computer screen on the clinical floors.
Second, hematologists are specialists just like any other practicing clinician. They know their stuff! They manage patient diagnosis, treatment, and follow-up with the most up to date literature, national cancer guidelines, and anything else available to better their patients’ outcomes. Despite the notes in the CBC results that there are numerous macrocytes with hypersegmented neutrophils, or 3+ schistocytes reported in a manual differential—seeing is believing. It helps to see the slide yourself and get a feel for the disease “state” with your own eyes. Moreso, it could be a learning opportunity. It’s well within a clinicians’ scope to come down and look at a peripheral smear, I actually encourage it. But it should come with a few caveats…I’ll get to those too…
I-CARE
One of the places I was proud to hang my lab coat was actually my first job as an assistant lab technician in the blood bank at Rush University Medical Center in Chicago. Before I got my MLS and way before grad school or med school, I was a blood bank “expediter.” Super fancy title, but all I did was make sure specimens were logged in and blood products were up to par with labels on their way out. Clerical but critical! (Let me have this, please…haha) Anyway, part of the culture at that hospital has stayed with me all these years. I’ve talked before about culture and the way it permeates an institution’s practice like at the Mayo Clinic, but for my first foray into clinical work their acronym was clutch: I CARE.
- I for innovation
- C for collaboration
- A for accountability
- R for respect and
- E for excellence
Why am I telling you this? No, there are no royalties. I just think it’s an easy way to remind ourselves about the meaning of interdisciplinary medicine and they way we should work together across specialties, and from bench to bedside. When we incorporate those values into our work for the purpose of improving patient care and outcomes, everyone wins. In this case, effective utilization of resources tells us that peripheral slide review means different things to different people. In the setting of hematologic work-ups, flags and review at the bench can signal something to the clinician which could spark a conversation with the pathologist. All parts contributing to a whole of patient care. Vigilante medicine is bad news. Collaboration is key.
One place I was lucky enough to be a part of this interdisciplinary collaboration was Swedish Covenant Hospital. One of the hematology physicians would routinely call me and ask to look as peripheral smears down in the lab, often as a group with med students, residents, and fellows. I’d throw the image of his patients’ slides on a large flat screen and go over what certain traits meant with regard to morphology and identification from the lab setting. Dr. Cilley would add what this all meant clinically and discuss treatment algorithms and next steps. That was collaboration at it’s finest: lab tech working with pathologists, clinicians working with the lab, and patient’s benefiting from all of it.
Teamwork makes the dream work
About those caveats for collaboration I mentioned earlier… Let me put it briefly: it’s well within the scope of a clinician to come over to the laboratory and get some information on their patient’s lab results/testing. But why not consider the following:
- If a physician calls to review a smear, offer to go over it with them. Likewise, to our clinical friends: if you go to the lab for a slide don’t be batman—ask the tech what they think!
Experienced techs are one of the hospital’s most valuable resources. Some folks I’ve worked with have been looking at slides longer than I’ve been using my eyes at all! They’ll save you and your residents the time when those terrifying intracellular microorganisms are really just overlying platelets. I mean, they’ve got a cute halo.
- If you need help, just ask. This applies to everyone.
Talking with the tech about the slide is great start, but there’s more resources in the lab than most people know what to do with! Clinical physicians: check the shelves around the hematology microscope. Stuck on something? Find a CAP atlas or a proficiency survey booklet guide. Easy to read. Techs and pathologists: have someone who constantly comes down for slide review despite your immaculate and detailed SOPs on CBC results reporting? Have a quick chat about the work that goes into resulting those diffs—you might even improve your heme TAT, who knows?
- If it’s well within the right of a physician to leave the unit and see a patient’s slide, logic says that maybe, just maybe, it should be okay for a pathologist to leave the lab and see a patient at the bedside!
Hospitals are full of never-ending rounding white coats, all asking patients questions, and all contributing specialty notes to their charts. But its not only to prevent patients from getting a decent nap. We’re all parts of a large interdisciplinary patient team. A recent Medscape survey found that somewhere around 3% of pathologists see patients, routinely! Got an interesting case in the lab, someone who’s part of lots of tumor boards, someone with an interesting case to write up, or even someone who nobody knows exactly what’s going on with? Try walking over to 4 south and have a conversation with Mr. Jones; it might help. At least he’ll know how many people are working on his care team!
The bottom line: we’re in this together, and like the flag on the ASCP ship says, we’re Stronger Together. Innovation, collaboration, accountability, respect, and excellence are—and should be—simple cornerstones of clinical medicine that translate across every discipline. When we share information and expertise, everyone gets better at what they do.
Thanks for reading!
See you next time!

–Constantine E. Kanakis MSc, MLS (ASCP)CM graduated from Loyola University Chicago with a BS in Molecular Biology and Bioethics and then Rush University with an MS in Medical Laboratory Science. He is currently a medical student actively involved in public health and laboratory medicine, conducting clinicals at Bronx-Care Hospital Center in New York City.