When I started my professional life, nobody talked about generations. Experience was everything: none, little, some, significant or expert. Now, conversations about generational similarities and differences are integrated into professional and personal life.
There are currently five generations at work today: Traditionalists, Baby Boomers, Generation X, Generation Y/Millennials, and Generation Z.

Understanding generations allows people to adapt their behavior according to certain preferences.Take, for example, communication styles. When communicating with someone from the Baby Boomers generation, picking up the phone might be appreciated, while sending an email to a Generation X is the best way to communicate with them. Always keep in mind, however, that generational preferences are generalizations, and knowledge about them does not substitute understanding each employee and colleague on an individual basis.
Another example of the differences between the generations is how they define their aspirations. Traditionalists value home ownership, Baby Boomers want job security, Generation X aspires to achieve work-life balance, Generation Y prefers flexibility and freedom, and Generation Z values security and stability. Understanding each generation’s aspirations allows leaders to tailor their communication style and job aspects to each individual.

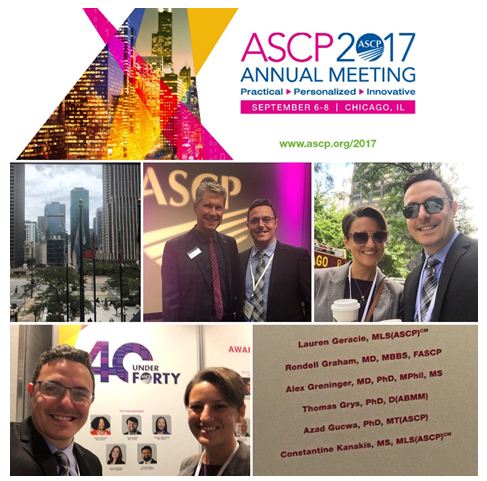
-Lotte Mulder earned her Master’s of Education from the Harvard Graduate School of Education in 2013, where she focused on Leadership and Group Development. She’s currently working toward a PhD in Organizational Leadership. At ASCP, Lotte designs and facilitates the ASCP Leadership Institute, an online leadership certificate program. She has also built ASCP’s first patient ambassador program, called Patient Champions, which leverages patient stories as they relate to the value of the lab.
As a former member of the ASCP Resident Council, I volunteered for the opportunity to serve as a beta tester for the ASCP Leadership Institute. To obtain certification, I completed 10 modules which often included a pre-course reading or interactive video assignment along with a pre-recorded webinar, post-test, and post-course evaluation. Some of these courses are also available in-person at live meetings and can include personal coaching live, online, or by phone.
A cursory internet search will reveal a plethora of written and video resources available on the topic of leadership. Additionally, many of us have participated in evaluations or trainings that sought to not only define our personal leadership skills/style but also help us to gain essential self-awareness and skills to better lead or be part of a team. Despite such experiences and even though I’ve held many leadership positions over the years, I still find it difficult to reconcile what it means to be a leader, both in terms of expectations that I hold for myself and those that others hold of me and how to build these expectations to realize a shared objective.
I was intrigued by the title of the module “DeCoding Generations”. This module was especially salient for me since I was a non-traditional medical student after initially studying to be a neuroscientist. I’ve generally been older than my fellow trainees and younger than the majority of my teachers. This generational gap has also been similarly evident within the teams I’ve participated in since I matriculated into medical school.
This module explored the core values of the following “generations”: traditionalists, baby boomers, gen X, gen Y (also known as millennials), and gen Z to help the learner understand what drives members of each group. The course then further defined the aspirations, attitudes toward technology and their careers, and preferred communication media and preferences of members of each generation. This was all with the goal of facilitating interactions, especially as a leader, with members from each generation. For instance, different generations prefer and respond better to different types of communication: in-person, phone, email, video conferencing, text, or a combination of these modalities. That’s where the “decoding” part of the module comes in. As leaders, we need to recognize how best to interact with each team member to acknowledge their core values and foster the most harmonious working relationships while working toward a shared goal.
I’m a very visual learner and intuitive person but not the most eloquent or at ease with verbal communication despite friends remarking that I’m a “social butterfly”. This module helped me evaluate ways to adapt my communication style especially when interacting with others in the two most numerous generations in the workforce: millennials (42%) and baby boomers (29%). I fall in the middle as a gen X’er (23%) and have often found myself confounded by the attitudes and behaviors of millennials and this module helped me to understand their perspective and preferred modes of communication. But what I learned most was to look at not only the differences that impair our interactions but also the similarities we share that can be used to prevent or resolve conflicts and to encourage team creativity and solidarity.
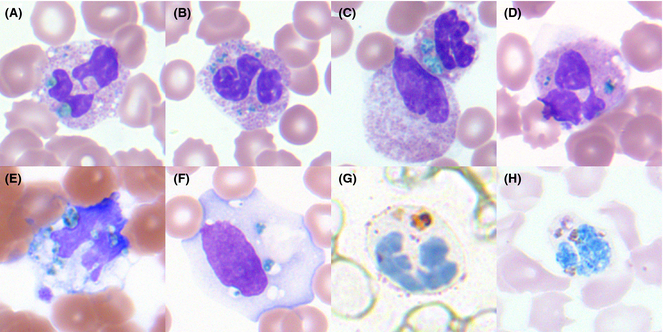
-Betty Chung, DO, MPH, MA recieved a BA from The University of Chicago, MA from Boston University School of Medicine, DO from UMDNJ-School of Osteopathic Medicine (now Rowan-SOM), and MPH from Columbia University and a decade of experience in basic science research. She completed her AP/CP residency at the University of Illinois at Chicago (PGY1-2) and Rutgers Robert Wood Johnson Medical School (PGY3-4). Her current interests lie in graduate medical education, quality improvement, hematopathology, and molecular genetic pathology.