Margie had worked in the histology department for years. She never used the chemical fume hood when pouring formaldehyde, but lately she had been coughing quite a bit, so she decided it was time to use the hoods. Soon she would be diagnosed with lung cancer.
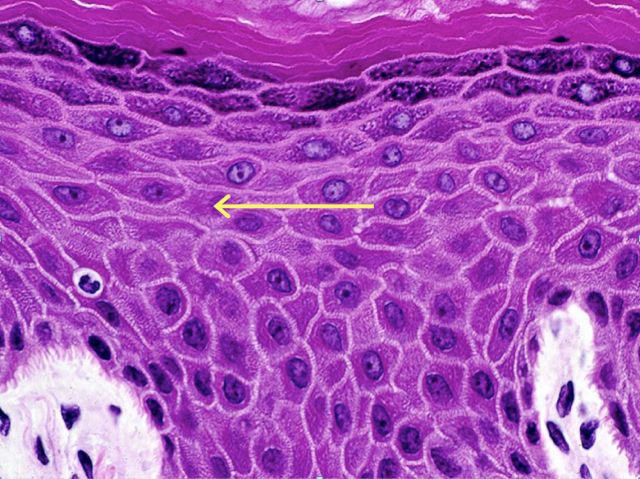
Steve was a cytotechnologist working in the radiology department for a fine needle aspirate procedure. The radiologist was in a hurry, and when he handed the uncapped sample needle to Steve, the needle pierced the skin in Steve’s hand. The patient had Hepatitis C.
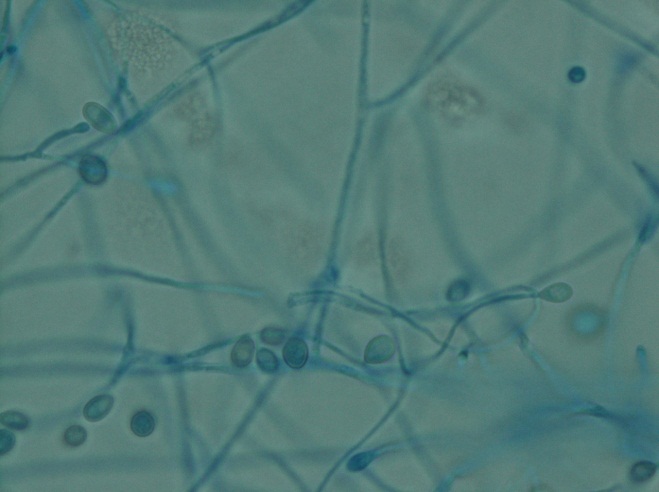
Jane had finished her long day of assisting with frozen sections and had to clean the cryostat. It was the end of the day, and she wanted to go home. She reached into the cryostat to change the blade with her gloved hands. She received a nasty cut on her finger, and since the blade had been used for multiple patients, Jane had to be treated for an exposure from an unknown source.
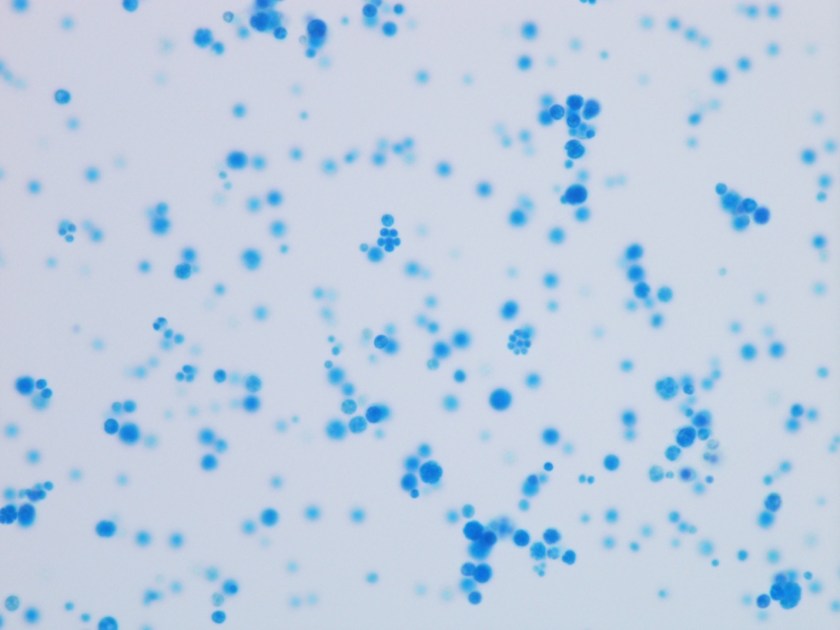
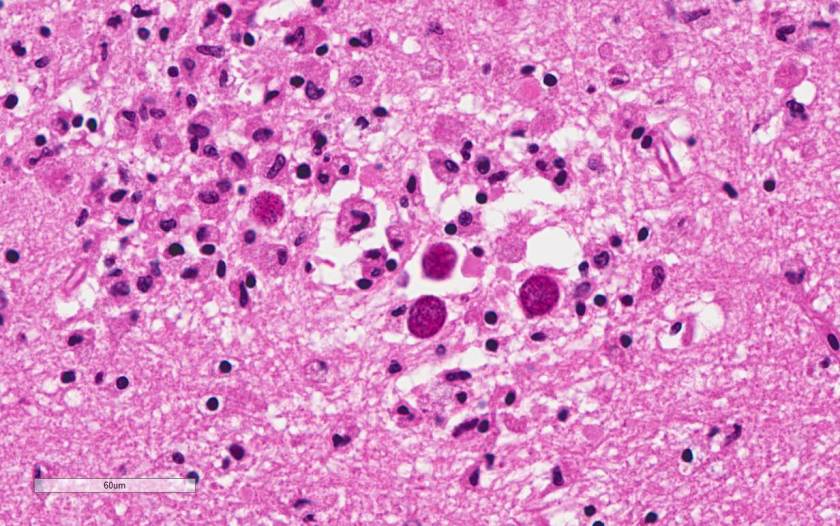
Anatomic Pathology laboratories present unique safety concerns that can differ from clinical lab concerns. Formaldehyde and other hazardous chemicals are used to preserve tissue specimens, workers can be exposed to large amounts of blood and body fluid during autopsies, and the sharp blades in cryostats and microtomes create additional cause for concern. Histology and Cytology employees need to be ever-vigilant to protect themselves from these exceptional hazards.
Formaldehyde and xylene are two chemicals typically handled in the AP lab. Xylene is a strong-smelling flammable liquid, and formaldehyde is listed by OSHA as a known carcinogen. If using these chemicals in the lab, you should have specific safety procedures for them, and vapor concentration monitoring should be performed to determine employee exposure levels. It is important to review the monitoring results as soon as possible, and never more than 10 ten days after receiving them. Discuss the results with each monitored employee individually or post the results in the department. Because monitoring is performed for tasks as well as locations, it is considered representative monitoring. That means one result may represent several employees who perform the same tasks or work in the same area.
If vapor concentration levels are elevated, make sure to take measures (such as using engineering controls) to reduce or eliminate staff exposure. OSHA’s Formaldehyde Standard requires annual monitoring if results are above the STEL (short term exposure limit). To discontinue sampling, the lab needs to obtain results from two consecutive sampling periods taken at least 7 days apart show that employee exposure is below the action level and the STEL.
OSHA requires a specific safety formaldehyde training for all employees who are exposed to formaldehyde concentrations of 0.1 parts per million (ppm) or greater. This formaldehyde training must include specific elements including education of the contents of the Formaldehyde Standard, the contents of the formaldehyde Safety Data Sheet (SDS), the health hazards of formaldehyde exposure, the proper use of necessary PPE, and spill response and clean-up procedures. This training is required by OSHA annually, and it may need to be provided to some employees who work outside the laboratory (operating room staff, labor and delivery staff, etc.). Even though the laboratory may not be responsible to provide this training, it is a good idea to communicate with other department leaders to ensure they get the required training for their staff.
Blades and other sharps pose great risks in AP procedure areas. Most microtomes and cryostats are equipped with knife guards- insist that they be used. Remove used blades with magnetic-tipped implements and insert new blades using rubber-tipped tweezers. Place disposable knives in sharps containers after use.
Odd as it may seem, there are Cytology procedures where the hand-off of uncapped needles containing samples sometimes occurs. Unprotected needles should never be passed from one person’s hand to another. These needles should be placed on a counter or the technologist should only take them from the collector with an implement such as tweezers. Be sure there is ample space to safely perform the cytology tasks in the procedure area away from the lab.
Laboratory Safety is not a “one-size fits all” umbrella for all areas where laboratorians work. Risk assessments and task assessments are critical to determine the particular hazards in a specific lab. In the Anatomic Pathology laboratory, these assessments should guide safety leaders to those specific safety measures which can help your staff prevent injuries and exposures which can be career and life-changing.

-Dan Scungio, MT(ASCP), SLS, CQA (ASQ) has over 25 years experience as a certified medical technologist. Today he is the Laboratory Safety Officer for Sentara Healthcare, a system of seven hospitals and over 20 laboratories and draw sites in the Tidewater area of Virginia. He is also known as Dan the Lab Safety Man, a lab safety consultant, educator, and trainer.