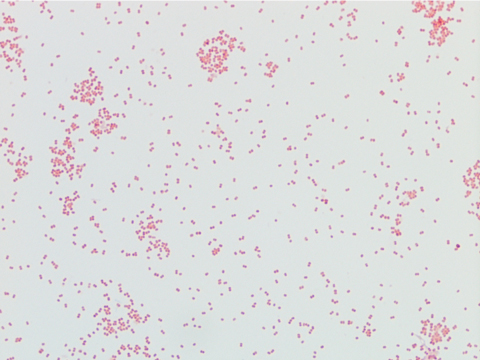
A recent report from the Centers for Disease Control (CDC) found that twenty-four laboratory workers were infected with a strain of Salmonella typhimurium, an enteric pathogen. The infections were reported in sixteen states across the country. Of those infected, six were hospitalized with symptoms such as diarrhea, fever, and severe abdominal cramps. Luckily, there were no deaths reported. These infections occurred in various teaching and clinical laboratories. The worst part? This could have been avoided.
When interviewed, some of those who became ill said they remembered specific exposure events. Many others who were unsure of how they became exposed described unsafe behaviors in the laboratory. Those victims admitted to working in the lab setting without lab coats or gloves, and many reported not washing their hands before leaving the department.
If you’re a laboratory leader, you very likely work during the day shift. Hopefully, when management is on site, staff is compliant with safety. If not, you may need to examine your safety program and leadership style. Do you enforce safety regulations in the lab? Do you lead by example? Do you don PPE when you pick up the phone or use a computer in the lab?
If safety seems to be good during the day, you may want to make a visit during the off-shifts. Depending on the level of safety culture, there may be anything happening from solid safe practices to open eating and drinking in the department. I know that was the norm in many labs 25 years ago, but those unsafe practices and safety violations should now be ancient history. Unfortunately, that is not the case, and that is one reason we have bacterial infection outbreaks in our laboratories.
An experienced lab auditor will tell you it is not difficult to assess the lab safety culture in a department, even on inspection day. I once entered a lab as part of an accreditation inspection team, and I watched as the lab staff struggled to find gloves. Even though they knew the inspection was imminent, they could not hide the fact that glove use was not the norm for them in that lab. A complete lab safety audit can reveal a number of inappropriate practices such as improper PPE use, gum chewing, cell phone use, and many others.
The National Institute for Occupational Safety and Health (NIOSH) has educated workers for years about hazard and exposure control. The “Hierarchy of Controls” is an excellent model to use in the laboratory setting, although certain facts about it may be surprising. The first and best two controls to remove hazards are elimination and substitution. Of course, these are not always possible in the lab setting. While there are substitutes for hazardous chemicals, the inherently dangerous specimens that are handled cannot be replaced or removed.
Engineering controls create physical barriers between the hazard and the employee. Biological Safety Cabinets (BSCs) and Chemical Fume Hoods are powerful engineering controls. Administrative and Work Practice controls are the safety policies and actual practices that help prevent infection. Written safety procedures are designed to change the way people work, and standard work practices include not eating or drinking in the lab setting and practicing hand hygiene when necessary.
The final control for infection prevention is Personal Protective Equipment (PPE). In the hierarchy, PPE is considered the last resort for staff protection. Since the lab hazard cannot be eliminated, and since humans commit errors with procedures, that final method of protection must be utilized. Lab coats, gloves and face protection need to be used at all times when working in the laboratory. Without it, the worker is at great risk for exposure- and that is what happened in the labs where the Salmonella infections occurred. Each of the controls that should be in effect in the lab were bypassed, and there were consequences.
It is always better to read about incidents that occur in other laboratories rather than have to report them about your own. When I hear of such stories, I always look at my own labs to see if such an event could occur there. What opportunities exist in my lab safety program? What about yours? Be sure to learn from these unfortunate events and keep your own staff safe.
The personal (and probably painful) part of the infection outbreak was that these laboratory workers were infected on the job, and then they brought it home. The CDC report says nothing about infections being spread to family members or friends, but it certainly could have happened. If there are weaknesses in your lab safety program, what could your staff be bringing home? What infections or diseases could be spread because of unsafe work practices? Now is the time to take the lead for your safety program before such an event can occur. Bring safety home for your staff. Teach them and lead them so that the unsafe practices of the past turn into practices that keep everyone healthy into the future.

–Dan Scungio, MT(ASCP), SLS, CQA (ASQ) has over 25 years experience as a certified medical technologist. Today he is the Laboratory Safety Officer for Sentara Healthcare, a system of seven hospitals and over 20 laboratories and draw sites in the Tidewater area of Virginia. He is also known as Dan the Lab Safety Man, a lab safety consultant, educator, and trainer.