In the late 1990s—early 2000s—we were faced with a critical shortage of graduates in clinical/medical laboratory science, and we started evaluating the benefits of having our own program. Once we made the decision to seriously consider implementing our own program, I pitched a proposal for a blended model of curriculum delivery. My proposal was accepted by the Mayo Clinic School of Health Sciences as a pilot program to be supported by our newly created education technology center. Since our program and the education technology center were both new, we certainly experienced some growing pains. Also, had I known we’d have to reconstruct major elements of our online content every time we upgraded our content management system, I might have thought twice about it!
In the end, it was all worth it because today, we have an outstanding program built upon a solid foundation of both traditional and online content delivery that leverages our staff infrastructure and can be effectively managed and maintained over time.
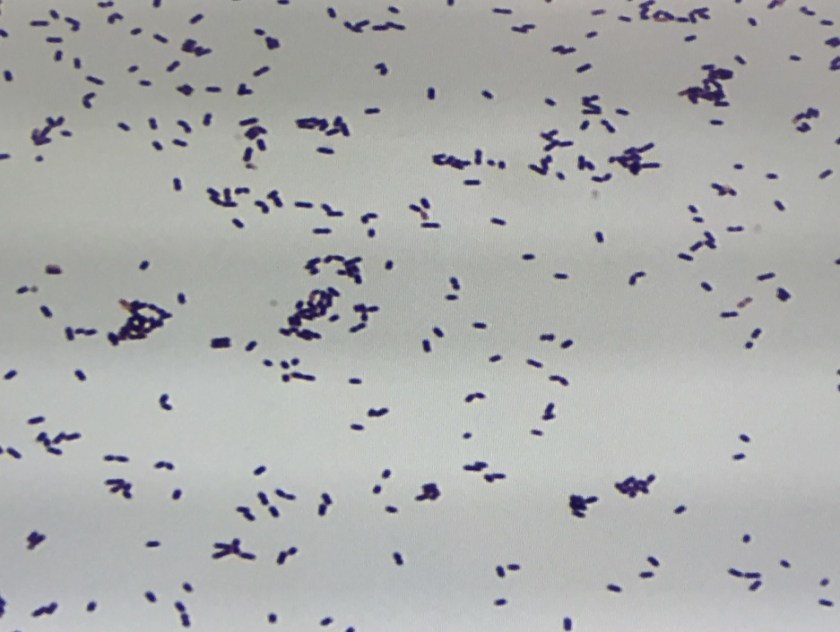
In the curricular model developed for our academic program in Medical Laboratory Science (MLS), the didactic component is provided in an e-learning platform (Blackboard Learn) and is underscored by Transactional Distance Theory (Moore, 1991), in which the three modalities of learner interaction with content, instructor, and fellow students are integrated into the online module. Each lesson plan includes a laboratory module taught by traditional methods of interaction between the instructor and student in a classroom setting. A constructivist learning environment is facilitated, and each lesson plan is closely anchored in the context of the work the student will perform upon employment.
Here is a simple diagram of our curricular model:

The following learning theories define our program curricular model:
- Transactional Distance Theory (e-learning theory): The online lesson plan includes learner-content interaction, learner-learner interaction, and learner-instructor interaction.
- Constructivism: The roles of both the teacher and student are redefined in this educational model. The teacher moves away from the traditional role of “sage on stage” to that of a “facilitator” of the student’s acquisition of knowledge. The student becomes a more active learner in this model, moving away from the traditional role of passive learner.
- Anchored Learning:
- Information is taught in the context of how the learner will apply it once he or she is working.
- The online homework lesson correlates with a hands-on laboratory lesson designed to reinforce the e-learning content.
- Reversing the Lecture-Homework Paradigm (Moses, 2002): The traditionally taught lecture is provided as an online homework assignment.
Embracing technology has provided a means by which we can improve our teaching methods and promote change in our education infrastructure. More than half of our didactic courses in our MLS Program apply the new education strategy I learned about as “reversing the lecture-homework paradigm” (more commonly known as “flipping the classroom”). Instead of going to lecture, our students complete web-supported didactic modules asynchronously as “homework” assignments, allowing more classroom time for laboratory instruction.
By providing more hands-on laboratory lessons, we are giving our students the opportunity to practice laboratory procedures and apply new learning material in a way that corresponds more closely with what they will do for a living after they graduate. Instead of giving the typical “one-directional lecture” with limited opportunity for dialogue, our instructors are able to spend more time with our students, teaching practical applications of the content, answering questions, and helping problem-solve.
References
- Moore, M. G. (1991). Editorial: Distance education theory. American Journal of Distance Education, 5(3), 1-6.
- Moses, G. A. (2002). e-Technology must enable big education goals. Proceedings of the 2002 e-Technologies in Engineering Education (eTEE) Conference, Switzerland, Vol. P01, Article 20, 142-145.

-Susan M. Lehman, MA, MT(ASCP)SM graduated from the University of Wisconsin-Madison in 1983 with a BS in medical technology. She is program director for the Medical Laboratory Science Program and course director for Clinical Microbiology I and II; her areas of interest include distance education and education methodology.