Hello again! Welcome back to my latest check-in following my progress with Zika risk reduction and public health outreach. Partnering with the Sint Maarten Ministry of Health through my medical school has provided amazing resources to take a look at social determinants of risk under the purview of public health, integrating both medical sciences and community service.
Early on in this project, I discussed the early stages in conceiving and planning these public health works in my first post “An Arbovirus Abroad.” This of course seemed like the perfect name for the proposal my team and I authored at the end of our first semester together. Done under an elective service credit, our full Internal Review Board (IRB) proposal for research within the community was called “An Arbovirus Abroad: a Service Learning Project Exploring Public Health Outreach, Social Determinants of Health, and Partnerships with Local Government to Address Zika Virus Knowledge and Community Outcomes.” The goals were to strengthen our partnership with local government offices as we aligned our efforts with reducing infectious risk and addressing community knowledge and attitudes regarding Zika.
Figure 1. Title Page of original IRB/Research Project Proposal under G. Jackson, Ph.D., Assistant Dean, Community Affairs and Service Learning at AUC School of Medicine
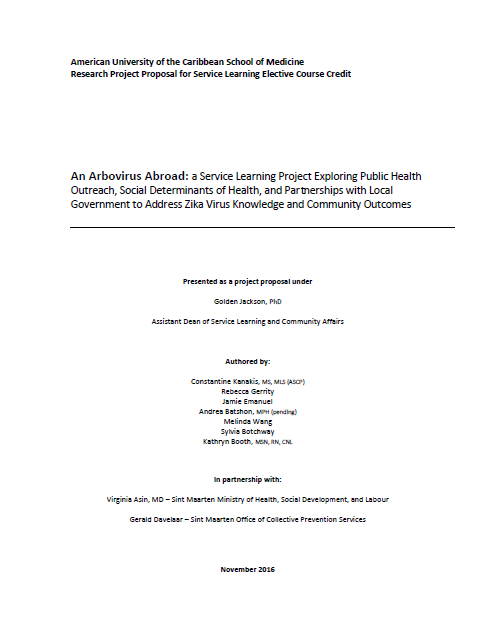
After we secured IRB approval, we began work quickly. Holding meetings with the Ministry’s representative consultant for their office of Collective Prevention Services (i.e. vector control) and scheduling the remaining work for the semester. With five new members of the “Z-Pack” we established a loose timeline with our advisor. Our new goal: integrate what we learned last semester and bring it to a conclusive change within the community.
Figure 2. Title card from initial briefing meeting with members of the Z-Pack, including coordinating partner from the Ministry of Health (CPS office) Mr. G. Davelaar.
This integration of knowledge from literature review/research, evidence-based best practices, and forward moving progress are all things those of us in the medical laboratory profession are quite familiar with. Getting IRB approval for a lab-centric project is quite involved and requires meticulous proof and substantial support to posit any claim to the benefit/risk ratio involved with human or animal subjects. I remember from my own graduate and undergraduate research that without heaps of evidence, you will be hard pressed to continue in any direction. While public health is a different science, the basis on evidence-based research is still present. During our initial assessments, literature reviews, and brainstorming, the “Z-Pack” went through hundreds of scientific articles covering everything from infection control precedents, to social behavioral change, and even the use of media and fear to illicit change.
Laboratory scientists know the impact of their work, though it may not always be the most evident to the general public. The near 70% of diagnostic information that comes from our work, and the virtual entirety of neoplastic diagnoses rely heavily on our training, skill, and certified competency in evidence-based practices. ASCP has a long-standing mission of advocacy for patients in the way its members and affiliates represent the profession at large. I believe that having those years of experience under my belt and those letters behind my name give me a head start when executing translational research. Going from raw data, analyzing it, and bringing it to life is something we all inherently train to do—and do well!
So, up to date, my team has secured two measures to contribute to our research. First, we gave an educational presentation to a community after-school program in one of Sint Maarten’s endemic regions. We had tailored a wonderful presentation I discussed in a previous post which caught the eye of the Ministry of Health and has spread to numerous places around the island under their sponsorship. With the same success, we managed to reach school-aged children in an engaging way about Zika, their health, and source reduction. Our second event is slated for this weekend where we have partnered with the Muslim student-interest group (MSA) on campus to go with them on their routine visit to a local mosque on a school-sponsored student service day we call “Community Action Day.” While the MSA students engage with their local community, the “Z-Pack” will conduct a two-part effort: to conduct a grounds-inspection for source/vector control around the mosque, and deliver a presentation for both children and adults regarding Zika prevention behavior.
How do those two events connect with my theme of evidence-based lab scientists? Well, one of my engagements when at Northwestern Medicine was to teach a course discussing transfusion protocols and laboratory information to clinical nursing staff. Presenting information, or teaching people, new ways to think about their environment at work or home is a part of being interdisciplinary. I was able to speak with medical jargon to the clinical staff, but with the children I have to use my ability in translating medical knowledge to understandable facts while also keeping the audience interested. My team proved in our last school-aged project, that when children are engaged and enthusiastic about something they have learned, they will take those messages home with them and hopefully contribute to a positive outcome. As for the second example, what could be more directly appropriate for lab folks to understand here: a surprise inspection! Sure, no one’s losing any accreditation points here, but the fact remains that we all have experience from one side or another making sure that things are up to code on pre-determined conditions and protocols. We have an SOP from the Ministry regarding the items of inspections as they relate to source control, so translating them to a new site should prove interesting.
I’ll close this post off with an interesting piece recently posted by Ms. Susan M. Lehman, MA, MT (ASCP)SM where she discussed learner (i.e. student) experiences. She talked briefly about how online curriculums and other lab-skills courses may rely on more independent learning, changing the expectations of students. One of her students summarized it positively saying, “you get what you put into it.” That’s what I think about the service elective my work is associated with. It could be simple directed readings with great discussions, but what my “Z-Pack” team has and the skills we each bring to it have made the project and its partnerships exciting.
Thanks for reading!

–Constantine E. Kanakis MSc, MLS (ASCP)CM graduated from Loyola University Chicago with a BS in Molecular Biology and Bioethics and then Rush University with an MS in Medical Laboratory Science. He is currently a medical student at the American University of the Caribbean and actively involved with local public health.