The manager walked into the lab to talk to Joan about the schedule. Joan was working with Mike, an older technologist who never seemed to follow the safety regulations of the laboratory. Joan was glad her manager was coming, because today Mike was wearing mesh sneakers and he was chewing gum! She couldn’t wait to see the manager chewing him out about that. However, the manager walked quickly to Joan, asked her a question and went immediately back to the office. She never said a word to Mike.
There are several things to be said about a scenario like this. First, why doesn’t Joan say something to Mike herself? Why doesn’t she feel empowered to speak up for safety? Has anyone ever taught her how to coach her peers for safety? Second, does the manager realize how much damage was just done to the lab’s safety culture? Intended or not, her ignoring Mike’s behavior is tantamount to permitting it, and therefore promoting it.
I was a laboratory manager before I became a Lab Safety Officer. When I moved to the safety role, I was lucky to have the previous safety officer still on site to provide orientation. As we walked through the labs, my predecessor noticed several safety issues and corrected them. I was very disheartened since I didn’t notice any of them myself. I wondered if I could do the job. Not long after that, I had a “safety epiphany.” I realized I could not see those safety issues because I had not trained myself to see them. I had not yet learned how to use my “Safety Eyes.”
Since then, I have been training lab people that “Safety Eyes” is a super-power that all laboratorians have. It is a latent ability and it must be honed in order for it to be effective. In order to do that, you need to know what to look for- be aware of the lab safety regulations so you can discern between right and wrong when it occurs. Next, you need to practice. That is the most effective development method for “Safety Eyes.” Knowing where to start can be difficult, so it is best to start by focusing on one safety topic at a time.
Begin by looking at Bloodborne Pathogens issues. For example, are people wearing correct PPE? Are waste receptacles properly labeled? Are spill kits in place and not expired? Next, look at chemical hygiene issues. Are secondary containers labeled correctly? Are acids and bases stored near the floor? There are a large variety of safety items under each topic that can be checked visually in the laboratory. Move to fire safety and on to other topics. Choose one area per week to start, and over time you will become proficient in spotting safety issues with your now-powerful “Safety Eyes.”
During the first year of my role as a Lab Safety Officer, I would become angry with the lab managers who didn’t seem to support the safety program- those who would walk through their labs and not see what I considered to be obvious safety issues. Then I had to remember my days as a manager- did I pay attention to those things? No, I didn’t. In part that was because I had so many things on my plate that I was focused elsewhere- just like the manager talking to Joan about the schedule. I also did not have any Safety Eyes training, so I simply wasn’t equipped to see all of the problems.
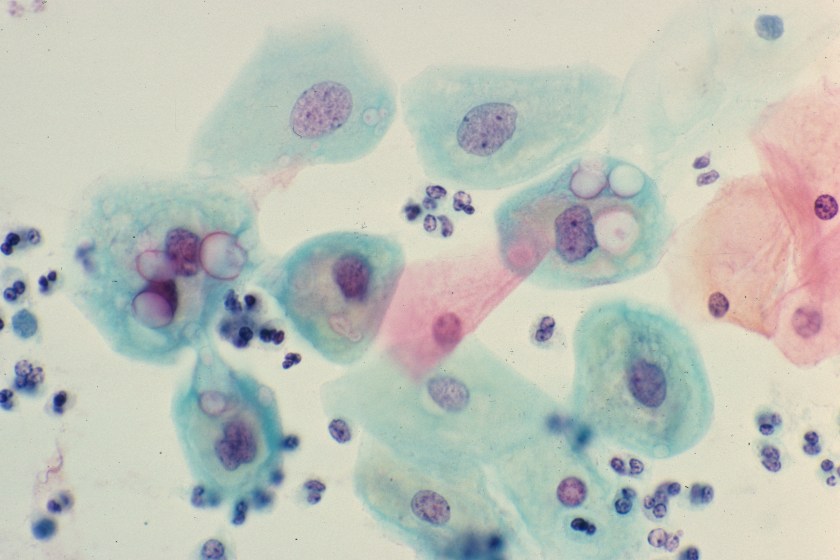
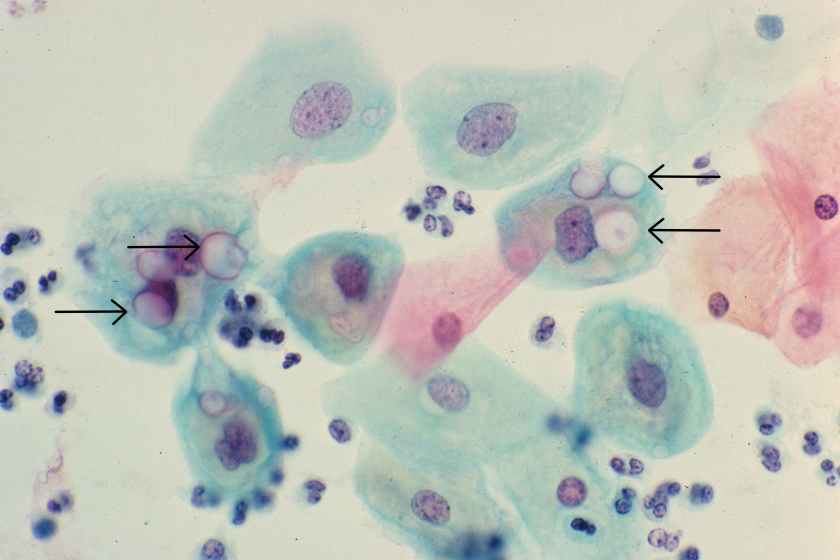
Today, I provide Safety Eyes training to lab managers. I use photographs of safety issues- pictures taken of real issues in the lab. Using these visual aids hones their ability to see the issues the next time they walk through the lab, and it raises safety awareness for everyone. If you lead a laboratory, and if you do not focus on safety, I understand that. However, you should understand that is important to make a change- develop those Safety Eyes and advance your safety culture in a way your staff can appreciate and support.

-Dan Scungio, MT(ASCP), SLS, CQA (ASQ) has over 25 years experience as a certified medical technologist. Today he is the Laboratory Safety Officer for Sentara Healthcare, a system of seven hospitals and over 20 laboratories and draw sites in the Tidewater area of Virginia. He is also known as Dan the Lab Safety Man, a lab safety consultant, educator, and trainer.