“Blotting,” in relation to molecular diagnostics, is a term that refers to the process of detecting the presence and quantity of DNA, RNA, or protein in cells. There are three main types of blotting procedures that those in the field should be familiar with: Southern, Northern, and Western. Three additional blotting procedures are termed Southwestern, Eastern, and Far-Eastern. These are also summarized in the table below.
Southern Blot Steps
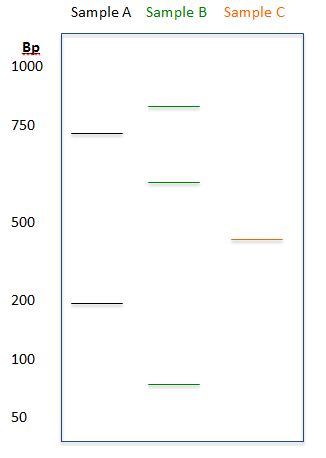
- DNA is isolated and cut with restriction enzymes.
- The DNA fragments are then analyzed by gel electrophoresis and separated by size (see previous blog post on Separation and Detection).
- Depurination – Gel is soaked in hydrogen chloride (HCl) to remove the purine bases from the sugar-phosphate backbone. This loosens up larger fragments before denaturation.
- Denaturation – The DNA is denatured by exposing the gel to sodium hydroxide (NaOH). Denaturation breaks the hydrogen bonds that hold the DNA strands together.
- Blotting – The denatured DNA is transferred to a solid substrate (nitrocellulose) that helps to facilitate probe binding and signal detection.
- Pre-hybridization – Prevents non-specific binding of the probe to other sites on the membrane surface.
- The membrane is exposed to the hybridization probe, usually a single DNA fragment with a specific sequence to the target DNA. The probe DNA is labelled either with radioactivity or fluorescent dyes.
Importance of the Membrane
Nitrocellulose and nylon membranes are best for smaller sized single stranded DNA fragments. It is compatible with many types of buffers and transfer systems. These membranes work well with protein and nucleic acids.
| METHODS OF TRANSFER | |
| Capillary Transfer | Utilizes capillary movement of the buffer from a soaked paper to the dry paper
Denatured DNA moves from the gel to the membrane |
| Electrophoretic Transfer | Electric current moves the DNA from the gel to the membrane |
| Vacuum Transfer | The force from suction moves the DNA from the gel to the membrane |
Northern Blots
Northern blots are used in the laboratory to look at RNA structure and quantity. It’s a powerful method that can measure levels of gene expression, as well as structural abnormalities in RNA.
- Needs to take place in an RNase-free environment.
- The samples are applied directly to an agarose gel.
- The sample is cut out from the gel, soaked in ammonium acetate to remove the denaturant (denaturant is inhibitory to the binding of RNA to nitrocellulose membranes), and stained with acridine orange or ethidium bromide.
Western Blots
Western blots detect proteins and separates them according to their molecular weight or charge
- Run using a polyacrylamide gel with molecular weight standards / markers.
- Utilizes capillary or electrophoretic transfer methods.
- Membrane must be blocked with a solution to prevent binding of the primary antibody probe to the membrane.
| TYPES OF PROBES | ||
| DNA Probes | Southern Blots | Complementary to the target gene |
| RNA Probes | Northern Blots | Complementary to the target sequence |
| Protein Probes | Western Blots | Antibodies bind to the target protein |
| SUMMARY OF HYBRIDIZATION TECHNIQUES | |||
| Method | Target | Probe | Purpose |
| Southern Blot | DNA | Nucleic Acid | · Gene structure |
| Northern Blot | RNA | Nucleic Acid | · RNA transcript structure, processing, and gene expression |
| Western Blot | Protein | Protein | · Protein processing and gene expression |
| Southwestern Blot | Protein | DNA | · DNA binding proteins and gene regulation |
| Eastern Blot | Protein | Protein | · Modification to western blot using enzymatic detection
· Detection of specific agriculturally important proteins |
| Far-Eastern Blot | Lipids | None | · Transfer of HPLC-separated lipids to PVDF membranes for analysis by mass spectrometry |

-LeAnne Noll, BS, MB(ASCP)CM is a molecular technologist in Wisconsin and was recognized as one of ASCP’s Top Five from the 40 Under Forty Program in 2015.