Have you ever felt like no one knows exactly what you do for a job; friends, family, even your colleagues? As a clinical pathologist, if you are ever asked what your job entails, it might take you a full 10 minutes to just explain the surface of it and by that time your audiences’ s eyes have glazed over and they are wondering when their next coffee break is. It can get pretty lonely when very few people understand your daily life of work.
I currently hold a general clinical pathology position and oversee the microbiology, chemistry, and immunology sections of a community hospital laboratory that services two hospitals totaling a little over 500 beds. I also get consulted on point of care testing and consult at two critical access hospitals that have a general AP/CP pathologist directing their lab.
As a new clinical pathologist, I was asked to blog about my experiences during the first year of working in the real world. I thought it would be a great venue to talk about how I have combatted the “loneliness” I face when I feel like no one knows what I do. Over the next couple of months I will highlight some of the tasks I have undertaken in my current position and I’d also love to hear what other clinical pathologist’s careers look like and/or how they have evolved over the years.
The beauty of a career in clinical pathology was explained to me by an attending during my residency training –you make of it what you want to. He also told me to not venture into the lab because they will ask you to do things, and since I am not very good at following advice, that is exactly the first topic I would like to explore: getting into the lab on a daily basis.
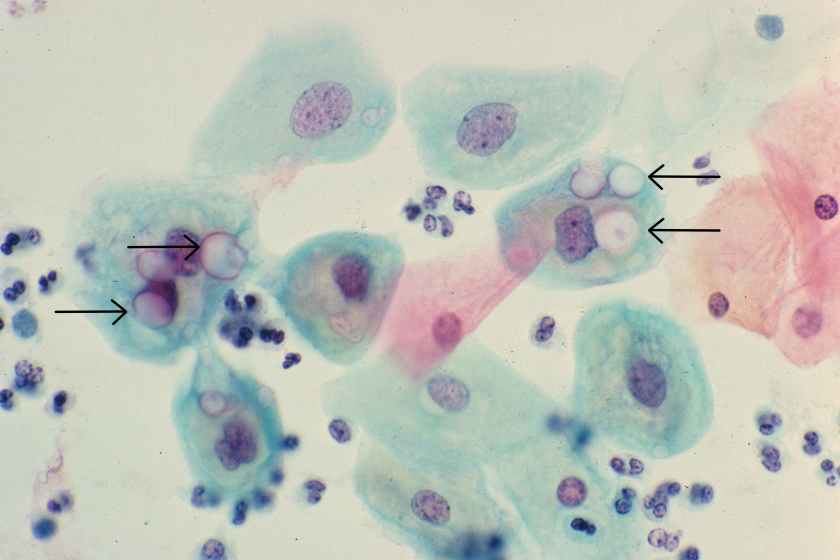
When I was in training, one of the best ideas I took away for my job was microbiology rounds. The first attending I observed holding these was a medical microbiologist that would round through the micro lab every day asking the techs if they had any odd cultures, questions that needed to be answered or anything that required follow up. When I took this job, I knew I wanted to incorporate this type of rounding as part of my work. My office is conveniently located at the back of the microbiology laboratory, so as I walk through the lab, I make it a point to say hi and ask the technologists if they have any issues, or any interesting cultures. It is not a formal rounding, but issues come out of these interactions and give me items to follow up with on a daily basis. Having my office located in the lab also allows the techs to come to me throughout the day with any questions they may have and has established a great rapport between us.
I also round through the chemistry and immunology section of the lab, specifically hitting second shift, as they lack a lot of interaction with clinicians. This has been a harder task for me because my subspecialty training was microbiology. I feel comfortable interacting with the technologists and lab staff, but when I first started I had the fear that I would not know the answer to a question I might be asked. Lucky for me, there are not as many questions that come out of these rounds. But of the questions I have gotten and I did not know the answer, it has never been a problem by me saying “I don’t know off the top of my head, but let me get back to you”. It also helps that I drop off candy in the break room while they wait on me – it is truly amazing how chocolate helps you make friends (thanks for the tip, Mindy Kaling). In addition to troubleshooting, rounding through the lab has given me the opportunity to interact with other people who have a passion for laboratory medicine. The techs will get just as excited about an interesting organism that was isolated or a new instrument we might bring in, and it is great to be able to share that passion you feel for your job with others.
Next month I will discuss a little more about the “formal” interactions I have set in the lab, but for now, let’s hear from you: how do you get involved in the lab and the technologists you work with?

-Lori Racsa, DO, is the director of microbiology, immunology, and chemistry at Unity Point Health Methodist, and a Clinical Assistant Professor at the University Of Illinois College Of Medicine at Peoria. While microbiology is her passion, has a keen interest in getting the laboratory involved as a key component of an interdisciplinary patient care team.