A 69 year old patient with cirrhosis presented to the ER with fever. Her bilirubin was markedly elevated at 7.4 g/dl and her hemoglobin and hematocrit were measured at 13.4 g/dl and 35.6% respectively with a MCV of 103.2 fl and MCH of 38.5 pg. The next day her H/H were 11.9 g/dl and 31.3 % respectively. While her hemoglobin one day later was 11.9 g/dl, the reported hematocrit was 39.3%. Patient had a bilirubin level of 8.7 g/dl at this time.
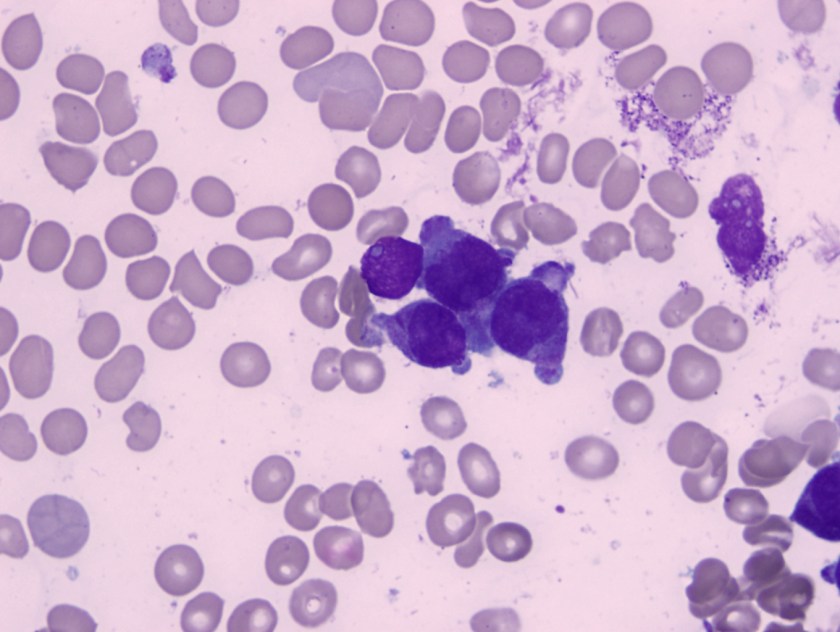
The fluctuating numbers together with the discrepancy between hemoglobin and hematocrit over a very short period of time was concerning. We realized that presence of markedly icteric plasma was responsible for these discordant values. Saline replacement and spun crit were performed in order to correct interference by bilirubin. Subsequent measurements of H/H revealed hemoglobin in the range of 12.9 g/dl with a hematocrit of 38% and a MCV of 113 fl. As the bilirubin levels started dropping (in the range of 6.5 g/dl) the hemoglobin level measured by the analyzer fell in the range of 10.3 to 11 g/dl. The instrument (XN-200) gave no error codes and therefore we were able to report out the analyzer results without correction. It was however very important to convey to the clinical team that the H/H values did not truly represent a fall from the previous values. As the two methodologies were different (spun crit and plasma replacement was being no longer performed) the numbers should be interpreted accordingly. Patient was not bleeding actively and did not require any blood transfusion.
Interference occurs when a substance or process falsely alters an assay result. Interferences are classified as endogenous or exogenous. Endogenous interference originates from substances present in the patient’s own specimen. Exogenous interferences are substances introduced into the patient’s specimen. Interference from hemolysis, icterus and lipemia are most frequently studied. Protein interferences are most often associated with paraproteins and predominantly with IgM or IgG and rarely with IgA. Drug interference may be due to the parent drug, metabolite(s) or additives in the drug preparation. Determining if interference is significant requires deviation limits from the original result. Once interferences are identified there is a need to establish procedures for handling affected results as part of the quality system.
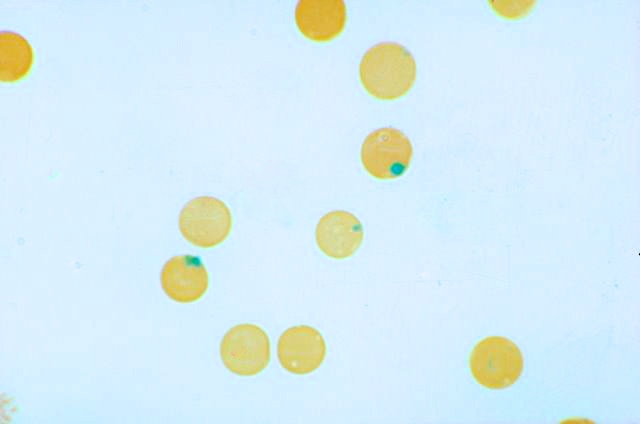
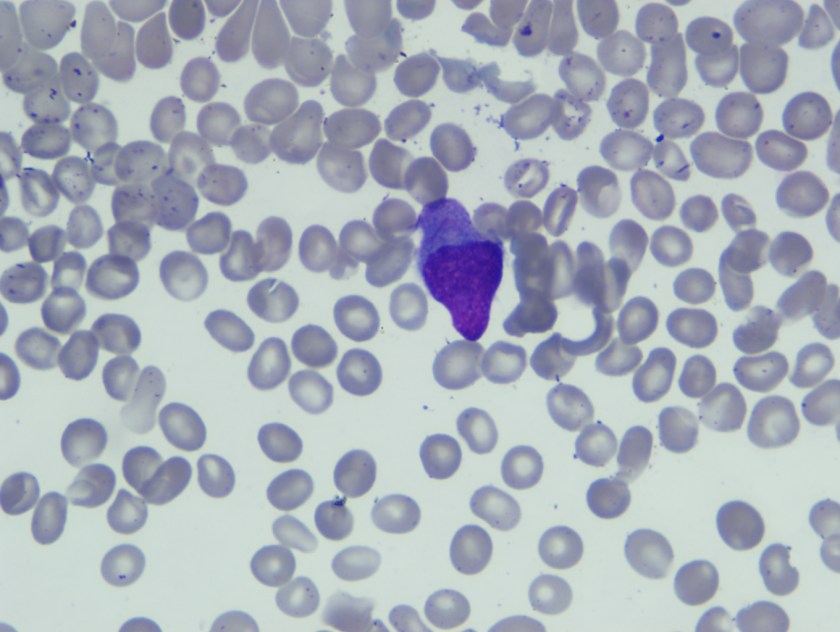
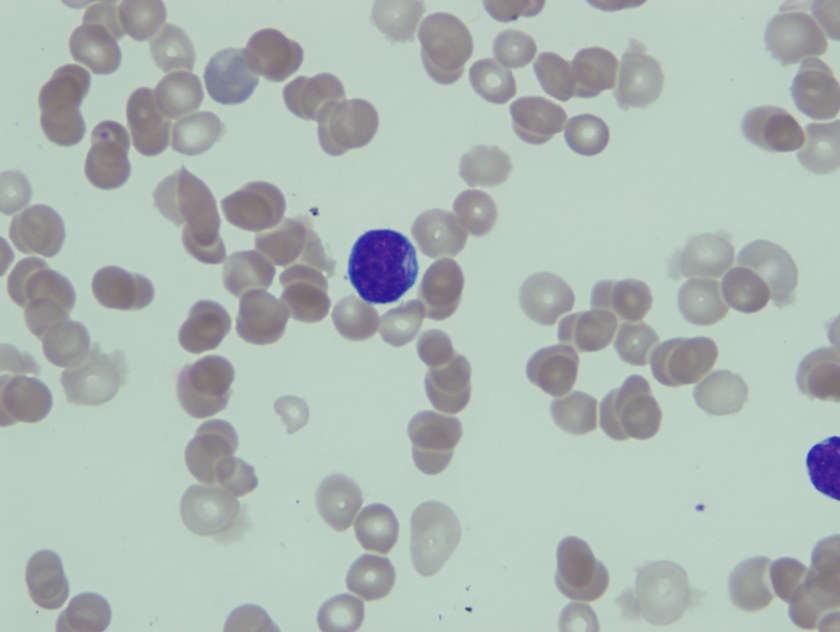
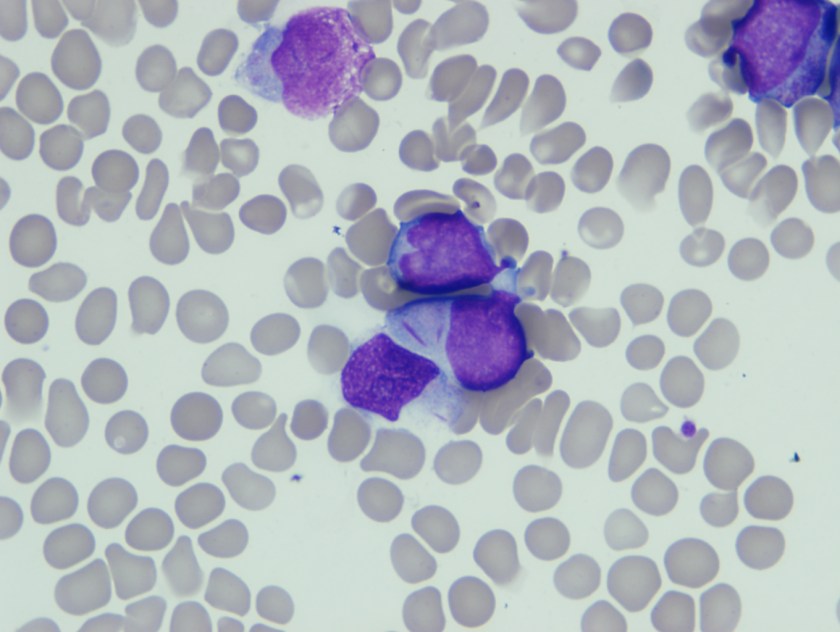
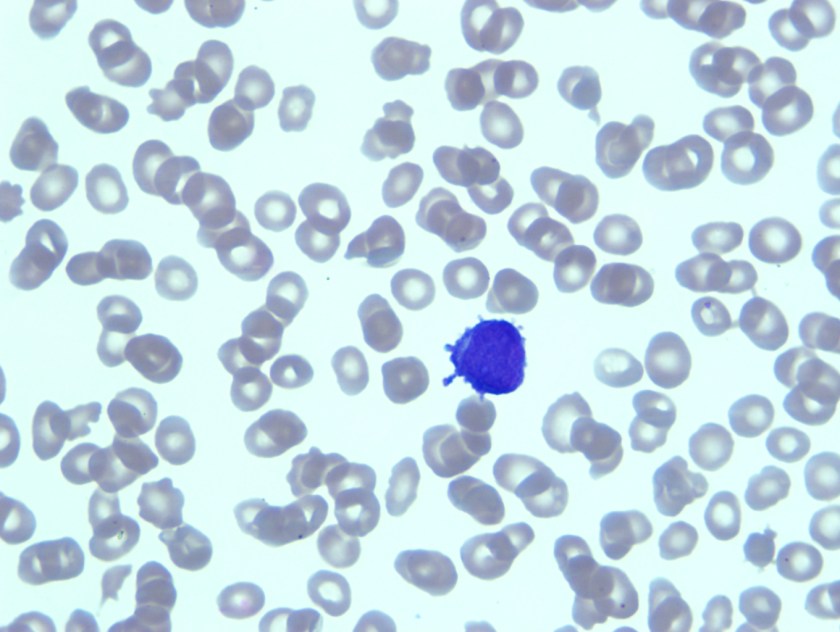
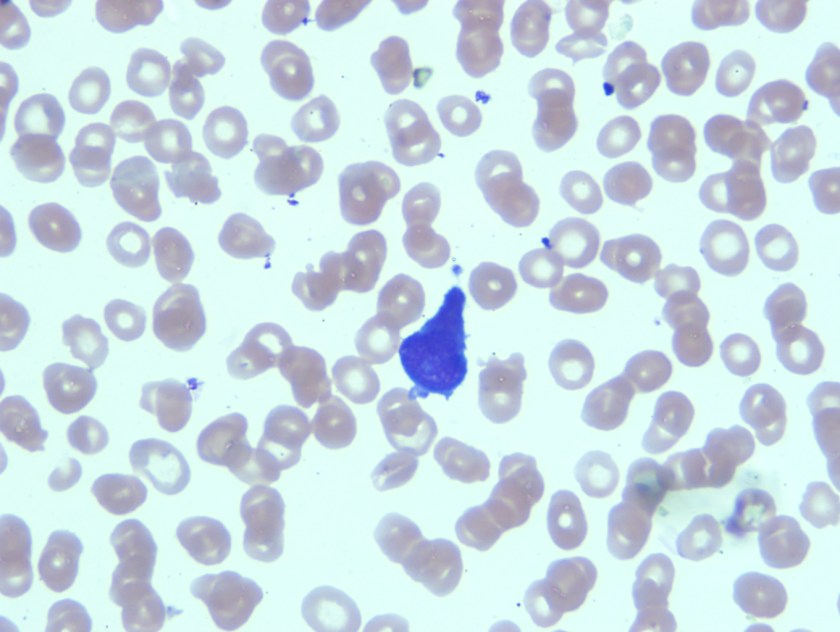
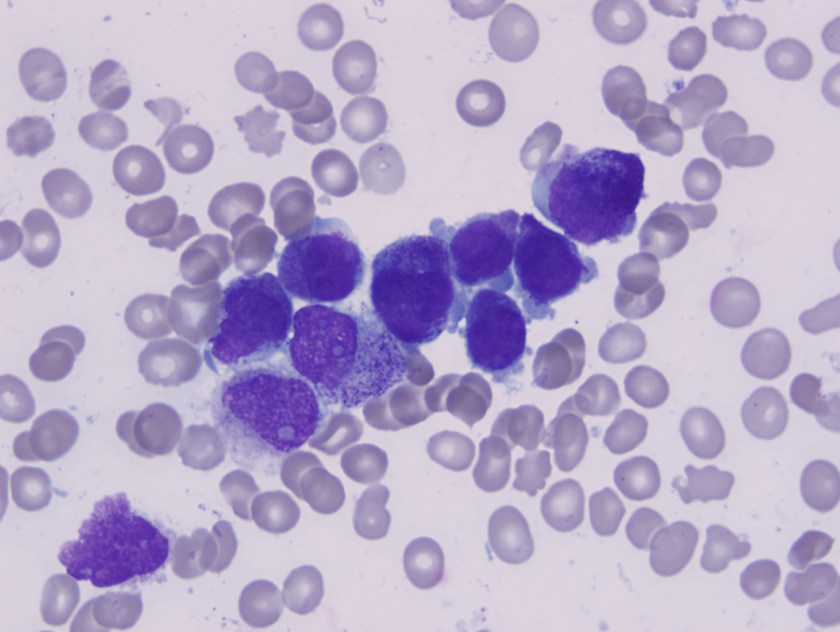
Hemoglobin is quantified based on its absorption characteristics. Conditions such as hyperlipidemias, hyperbilirubinemia, a very high white blood cell count, and high serum protein can interfere with this measurement and result in falsely elevated hemoglobin values. When the values of hemoglobin, red cell count, and MCV are affected, MCH and MCHC also become abnormal, since these indices are calculated and are not directly measured. Sometimes a set of spurious values may be the first clue to an otherwise unsuspected clinical condition (e.g., the combination of low hematocrit, normal hemoglobin, and high MCV and MCHC is characteristic of cold agglutinins).
Although one must pay attention to very high amounts of bilirubin within the plasma, most hematology analyzers do not presently demonstrate any interference with bilirubin, at least for concentrations up to 250 mg/l. Above these values attention is however needed.
High serum or plasma bilirubin concentrations can cause spectral interference with assays near the bilirubin absorbance peak of ~ 456 nm. Chemical interference e.g. with peroxidase-catalysed reactions may also occur.

-Neerja Vajpayee, MD, is the director of Clinical Pathology at Oneida Health Center in Oneida, New York and is actively involved in signing out surgical pathology and cytology cases in a community setting. Previously, she was on the faculty at SUNY Upstate for several years ( 2002-2016) where she was involved in diagnostic work and medical student/resident teaching.