The manager of the microbiology laboratory walked into the monthly staff meeting to discuss safety. Her first announcement was that the one clean hand washing sink in the department was going to be removed. The techs were shocked, and some were angry. Didn’t the manager care about infection prevention and control? Didn’t she know that hand hygiene should always occur after PPE is removed and before leaving the lab? The manager waited for the reactions to subside, then she explained that since the staff treated the lab as a clean area in many instances, that there should be no need for hand washing. The staff went on to argue that they were working with microbiological pathogens, and that they did wear lab coats and gloves, especially when handling specimens and setting them up for cultures. Some of those specimen containers were pretty disgusting, in fact.
That was when the manager dropped the charade. She had no real intention of removing the sink, but she wanted to make a point. She was tired of watching her staff reading culture plates with no gloves. She had spoken about it before, but no one agreed- they had been handling incubated plates for years.
One of the most common issues lab managers and safety professionals face is maintaining Personal Protective Equipment (PPE) compliance in the work area. An effective weapon in this battle is telling stories of lab incidents with bad outcomes, or explaining the consequences of this unsafe behavior. That is a valuable piece of lab safety education. It is unfortunate that we sometimes have to learn from others’ mistakes, but when it comes to safety, that’s better than learning from your own. Some lab accidents and exposures can be career-altering or career-ending.
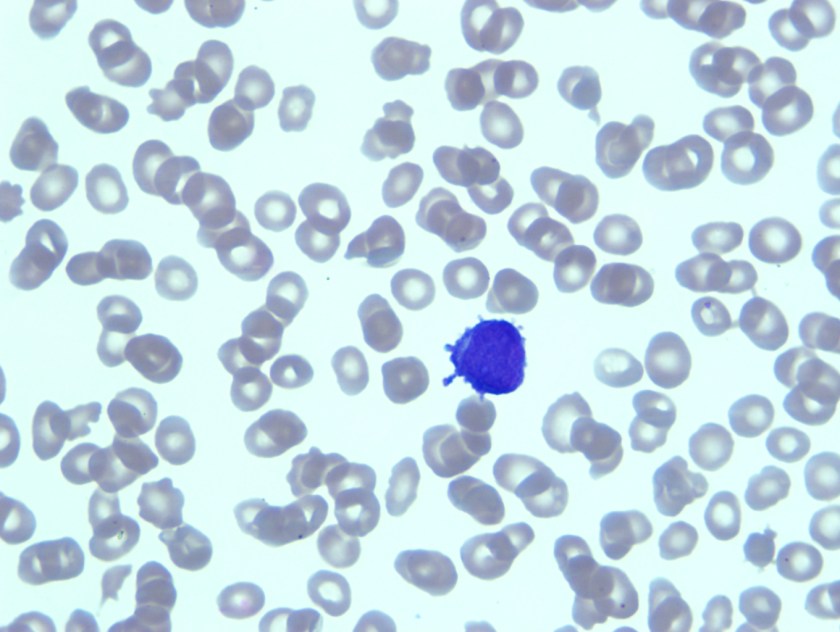
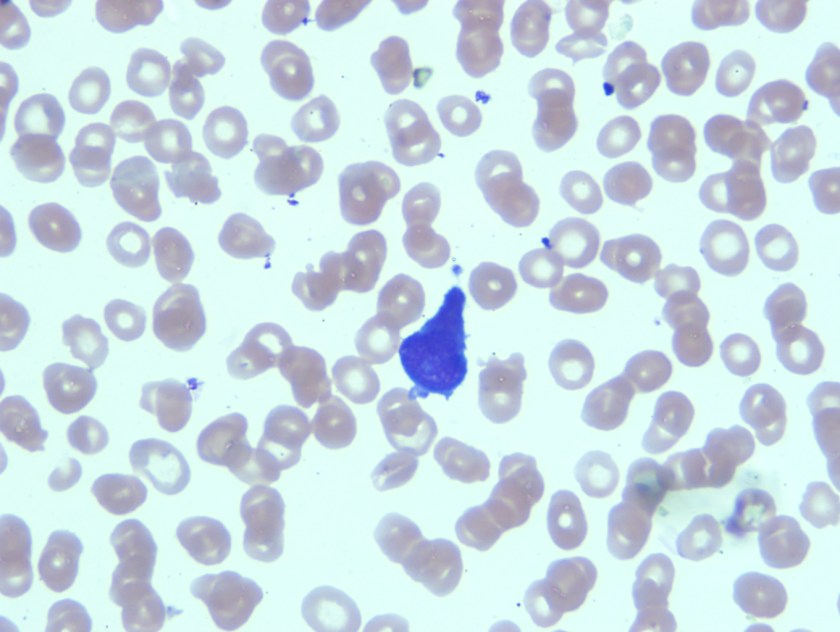
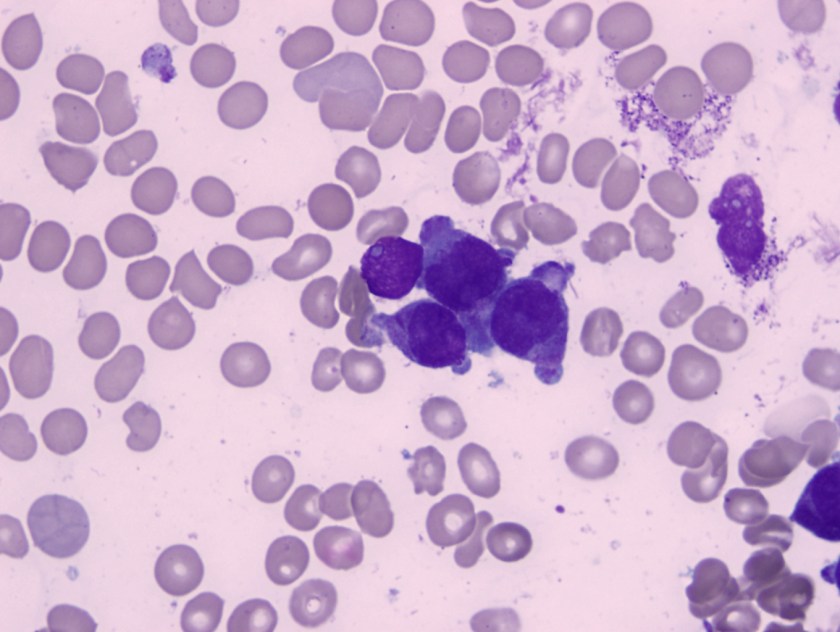
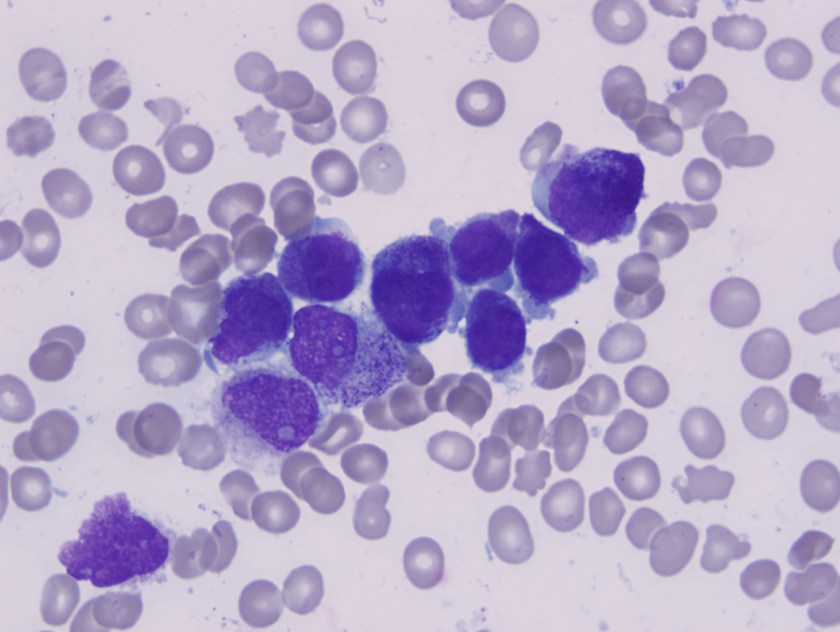
OSHA’s Bloodborne Pathogen Standard states that PPE (specifically gloves) must be worn when there is a risk of exposure. That is as specific as they get on the topic. Anytime patient specimens are handled or opened, it follows that gloves should be worn. That means that in the microbiology area, staff is handling specimens and agar plates with gloves while they streak plates and set up gram stain slides. These contaminated gloves are handling plate after plate, and then those plates are placed into the incubators. Like any other contaminated item in the lab, those plates should be treated and handled with gloves until properly discarded. That means that gloves are necessary when removing plates from the incubator, and when reading those cultures. Not only is staff handling contaminated plates, but they are working with bacterial and fungal colonies. There is a high risk of exposure in those processes.
OSHA also requires PPE under its Chemical Hygiene Standard (or Lab Standard). Gloves are required when handling chemicals, so they would be needed when performing simple chemical tests (oxidase, catalase, etc.) and when performing gram stains. Make sure you use chemical-resistant gloves when selecting the appropriate PPE for these tasks.
In 2010, OSHA responded to an inquiry specifically about the use of gloves while handling culture plates in the microbiology laboratory. The letter “strongly suggests” the use of gloves for the task, but OSHA’s own standards already address the issue and clearly require the need for PPE in that situation.
The story at the beginning of this entry is true- there was a lab manager who was fed up with her staff not wearing gloves, so she told them she was removing the sink. She was kidding, but she made her point. In that microbiology lab they all wear gloves to read cultures today.
Laboratory-acquired infections occur every year, and some of the easiest ones to investigate are the cases in which techs are infected with pathogenic bacteria. It is fairly easy to trace the sources of those exposures. What is the staff doing in your microbiology laboratory? Are they doing everything they can to prevent exposure to pathogens? As a manager or safety professional, are you enforcing the use of PPE when exposure is possible? Keep your staff from becoming a safety statistic- provide PPE, teach consequences of unsafe behaviors, and monitor the continual use of those safe work practices in your lab.

-Dan Scungio, MT(ASCP), SLS, CQA (ASQ) has over 25 years experience as a certified medical technologist. Today he is the Laboratory Safety Officer for Sentara Healthcare, a system of seven hospitals and over 20 laboratories and draw sites in the Tidewater area of Virginia. He is also known as Dan the Lab Safety Man, a lab safety consultant, educator, and trainer.