Hello again everyone! Welcome back.
No, I’m not talking about Netflix or HRH Queen Elizabeth II, nor am I making references to tiaras, bars, beer brands, or imminently deliverable babies…I am, of course, talking about Coronavirus as it would certainly have caught most of our collective attention in the media by now.
I really enjoyed writing last month’s list of what I think are important things on the horizon for pathology and laboratory medicine this new year, but this month let’s take a more topical turn. So put your surgical masks on, wash your hands, quarantine the next 10 minutes of your time and get ready as I take a shot at the novel 2019 coronavirus outbreak!
***Let’s talk about you and me, Let’s talk about COVID-19…***
Less-Than-Common Cold
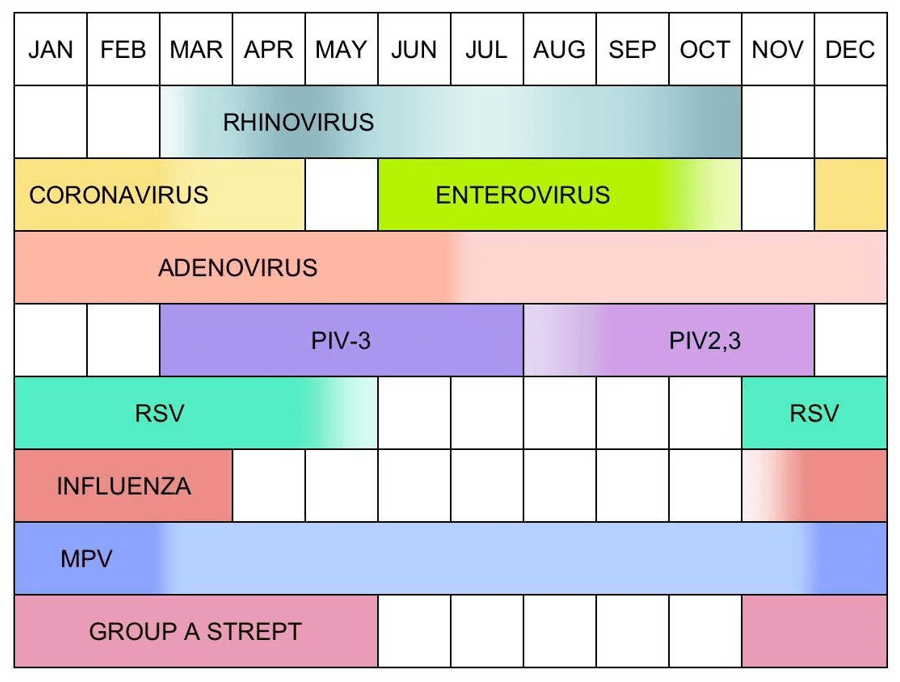
A long time ago, in a galaxy far, far away (aka: last year, about 20 minutes north of my apartment in Manhattan) I was in medical school, on rotations on the floors of a hospital in the Bronx. I experienced the surges of two flu-seasons and had a fantastic little mnemonic to remember the viruses that caused colds in most patients. Depending on age and immune system status, you had to think about the principal three viruses we see all the time—I remembered them as: “c-A-r,” note the capital “A.” Let me explain; the letters correspond to coronavirus, adenovirus, and rhinovirus. The are in a general order of when they appear during the months of the year (as coronavirus and rhinovirus kind of switch off in the spring, while adenovirus is around always thus is capital designation). There are a few hundred viruses which contribute to cold/flu-like symptoms in patients and, unless a patient is compromised in some way, we really worry most about one of them. Hint: it’s the one we give shots for annually, more on that in a minute.
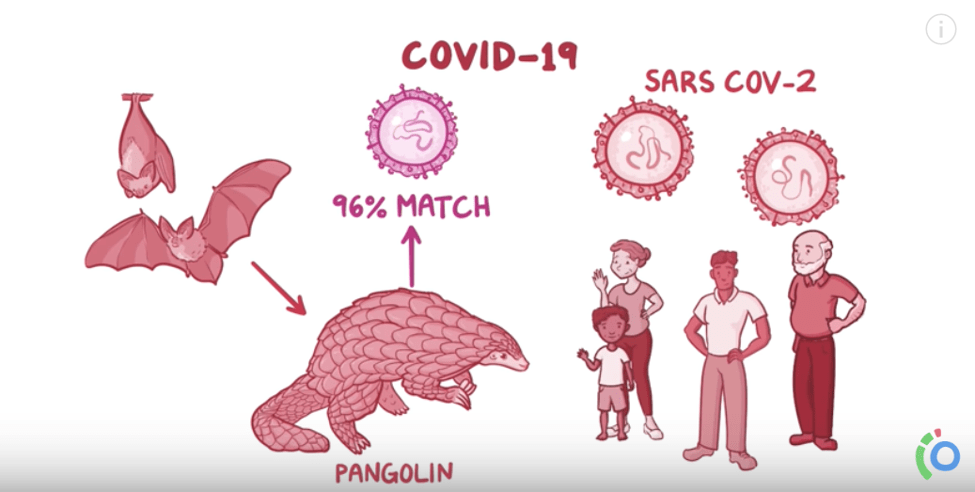
As far as this coronavirus outbreak is concerned, this is a “novel” (i.e. new) variant (read: mutation) of a respiratory viral pathogen that is affecting a disproportionate number of patients in higher severity than expected. Its official entity name has now been filed by the World Health Organization (WHO) as COVID-19—corona virus disease of 2019. The actual virus is a relative of the infamous SARS virus from the early 2000s. That was SARS, this is SARS 2.0—literally. This virus is designated SARS-CoV-2. SARS stands for Severe Acute Respiratory Syndrome and is caused by strains of coronavirus found in the remnants of infected individuals’ coughs and sneezes—please wash your hands—and causes a spectrum of symptoms from mild to severe including pneumonia, respiratory disease, and even renal failure.

How Does this Even Happen?
Okay, who took a sabbatical to Wuhan, China, and ate a wild fruit-bat salad? No one, that’s not how this works. But, if you’re looking for quick grocery store recommendations at the present moment I’d probably tell you to check out ALDI or a farmer’s market a few spots higher on the list than the Huanan Seafood Wholesale Market in Wuhan which harbored a majority of outbreak case-cause tracings. The bottom line is that COVID-19 and the SARS-CoV-2 have appeared in the world the same way the previous similar outbreaks have—through zoonotic mutations which then spread to humans. This zoonotic transmission is so effective to presenting humans with super infectious entities because it sends us pathogenic material we would have never seen before and our “naïve” immune systems are caught off guard. Now don’t get all panicky; yes, I’ve seen Contagion, Outbreak, and read The Andromeda Strain—in fact, I absolutely love when epidemiological medicine has the media spotlight. It’s a very exciting way to showcase public health, medicine, and—our favorite—laboratory professional work!
Basically, this process of mutation and transmission is the modus operendi of a viral particle. You can’t quite kill them, they’re not quite alive by biological definitions, they’re just packaged proteins on autopilot. They’re kind of like natural robots that want to propagate their species by adapting over time—they’re The Borg or Cybermen, depending on your sci-fi preferences. But both offending automaton predators have a mutual enemy in public health—a doctor (get it? TARDIS pilot and/or Beverly Crusher both work wonders in a pinch…) Anyway, it’s never just physicians, but a whole hard-working team of health advocates that conduct surveillance, field research, epidemiologic studies, and first-hand treatment.
***Side note: if you’re bored, in a hurry, or just don’t like my articles—don’t fret! Go watch that Osmosis video on COVID-19 and you’ll be up to snuff on the current outbreak in no time. Or in 12ish minutes.***
***Hey, you made it this far. Great! Interested to know more about the COVID-19 virus from our very own American Journal of Clinical Pathology? Visit here to learn more about the story of how this pesky coronavirus mutated its way into headlines. Fresh off the AJCP presses this month!***
You Should Update Your Antivirus Software
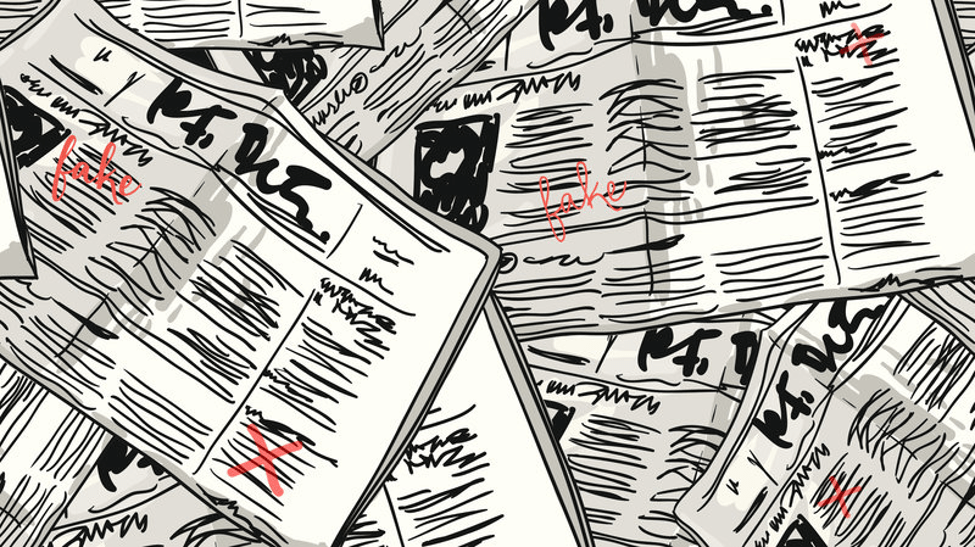

No doubt in my mind you’ve probably seen plenty of coverage about SARS-CoV-2 in the media. I’d also be willing to bet a lot of it is either dilute, sensational, or possibly even misleading. Regardless, there are always going to be people that don’t “buy in” to the public health message. If you remember Contagion¸ Jude Law’s character pushes the efficacy of “forsythia,” a homeopathic herb supplement that supposedly mitigates the horrible disease spread from southeastern Asia from improper food handling—if I recall correctly, it was a paramyxovirus that time. In this SARS-CoV-2 epidemic we have no current effective treatments, so prevention is key.
In an effort to address this type of health misinformation the WHO and CDC are actively disseminating as much educational information and graphics as they can write. Trying to dispense advice for the public including proper mask wearing, education videos, and myth-busting (i.e. hand dryers do NOT kill the COVID-19 virus, UV lamps do NOT kill the virus, thermal readers are effective in screening populations for symptoms within limitations, alcohol and chlorine do NOT kill the virus, receiving packages from China is still safe, pets don’t harbor the virus at this time, other vaccines do not affect this virus, saline nose sprays do not affect this virus, garlic/oils/other supplements have no effect on this virus, and all age groups are affected)—good stuff there. The most trusted sources of information regarding epidemics should be the representatives of functional medicine and health outcomes, doing work every day to make people healthier. Often times, politics, misinformation, or complex situations make information delivery harder than you’d think and the risks are increasingly high.
A Crown of Thorns: Don’t Forget About the FLU!
Flu vaccine deniers: turn away now or be healed! —or at least exposed to another point of view rooted in evidence-only concepts in medicine and population health. Consider the following: as of this month, COVID-19 has infected 43,000 people and killed 1,000 (approximately 2-3%). Remember SARS? That infected 8,000 and killed 700 (approximately 10%). MERS? 2,500 infected, 860 deaths (approximately 34%). And what about Ebola? 29,000 infectious cases with 11,000 deaths (approximately 40%). That was sourced from the Osmosis video with data from the WHO. Pretty impressive right? Well, not if you look at this: according to the CDC, the 2019-2020 influenza burden statistics include 36,000,000 infectious cases, with 17,000,000 clinical visits, 440,000 hospitalizations, and 36,000 deaths. One might say “hey, Dr. Kanakis, slow down there you’re spitting out all these numbers and the facts won’t lie. Looks like influenza only killed 0.1% of cases.” And you know what, you’re right. 0.1% is lower than the other viral epidemics. But check this out, because of the sheer number of cases, that means more people died of influenza than COVID-19, SARS, MERS, and Ebola COMBINED and those happened in other years. That‘s just this year’s flu season alone. I’ve talked before about recognizing and detecting the common cold vs. influenza before, check it out if you’d like a refresher!

We have influenza every single year, and it kills so many more people than we realize. If you want to talk about a terrifying, global viral epidemic, we’ve already got one. And it’s closer than you think. So wash your hands, reduce exposures if you’re sick or immunocompromised, get proper rest, eat well, exercise, read my articles every month, but most importantly—and I cannot stress this enough—get your FLU SHOT!
Thank you so much, see you next time!

–Constantine E. Kanakis MD, MSc, MLS (ASCP)CM completed his BS at Loyola University Chicago and his MS at Rush University. He writes about experiences through medical school through the lens of a medical lab scientist with interests in hematopathology, molecular, bioethics, transfusion medicine, and graphic medicine. He is currently a 2020 AP/CP Residency Applicant and actively involved in public health and education, advocating for visibility and advancement of pathology and lab medicine. Follow him on Twitter @CEKanakisMD
