Recently our lab was asked by physicians to start reporting band counts of ≧10% as critical values. While we have always reported bands when a manual differential is performed, we have also heard for years about other labs that have stopped reporting bands. Mayo Clinic stopped reporting bands in the 1990’s- other nationally and internationally known hospitals and community hospitals alike have followed suit. CAP proficiency surveys for cell ID do not separate segmented neutrophils and band neutrophils for cell IDs. Our hematology analyzer reports Immature granulocytes (IG) and we have learned about the benefits of IG over the band count. Thus, when our pathologists asked us to add a critical value for bandemia, we wondered if we were moving ‘backwards’.
Bandemia is defined as elevated band neutrophils in the peripheral blood. Neutrophils are produced to help fight infection. With infection, there is an increase in WBCs being released by the bone marrow into the peripheral blood. Bands are considered mature neutrophils and can fight infection, and in an effort to keep up with demand, some of these infection fighting cells which are released are bands. However, we are reminded that this is a nonspecific clinical finding. Bands can be elevated in many situations including inflammation, autoimmune disease, metabolic abnormalities, pregnancy, and treatment with granulocyte colony stimulating factors. Band counts of ≧10% have been used clinically as an indicator of serious bacterial illness. A finding of bandemia can help providers decide what steps need to be taken in evaluation of a patient, and in conjunction with clinical findings, can help in making a differential diagnosis.
The trouble with bands is that they are notoriously difficult to measure accurately and precisely. Bands are somewhat controversial and there are conflicting opinions on the utility of bands. Should bands be reported or included with neutrophils? A left shift reflects bone marrow response to bacterial infection, and this has been quantified as band count or immature granulocyte count. Is the IG a better parameter than the band count?
If your Hematology analyzer reports the absolute neutrophil count (ANC) with an automated differential, this includes all mature neutrophils. The theory that supports this is that neutrophilic bands and segmented neutrophils are both mature cells, and both fight infection. A true left shift would therefore be the presence of immature granulocytes (metamyelocytes, myelocytes and promyelocytes). Yet, we also now have analyzers that offer a 6-part differential that includes the immature granulocyte (IG) count. And we know that an automated differential is based on counting thousands of cells, and a manual differential is based on counting 100 cells. So, which is better? We can theorize that the IG is a better indicator of left shift because the automated diff count looks at more cells than a 100-cell manual diff.
Let’s say that we have a patient with a WBC of 20 x 103/μL. Left shift is defined as an absolute IG count >0.1 x 103/μL. Automated diffs can count >30,000 cells depending on the WBC count. If the auto diff counts 32,000 cells and finds 1% IG, this means that the analyzer identified 320 IG. Absolute counts are calculated as % x the WBC, in this case 0.01 x 20,000=.2 x 103/μL. This meets the definition of a left shift. If we do a manual diff and count 100 cells and see 1 meta, the absolute IG would be .2 x 103/μL, again meeting the criteria for a left shift. However, if we did not see any metas or other IG on the manual diff, the absolute IG would be 0. Thus, performing a manual diff, the difference in seeing 1 cell or 0 would make the difference of reporting a suspected infection versus no suspicion of infection.

With the advent of the IG count on automated differentials, labs have moved away from reporting bands. I have attended conferences and heard presentations about “banning” bands. A few years ago, I wrote a blog called “Beyond Bands: The Immature Granulocyte Count”, describing the benefits of using the IG count over bands in manual diffs. The above example would support “Ban the bands” arguments. Using the IG count from analyzers can take advantage of analyzing many more cells and give us statistically more precise values.
Results from auto diff can get to patients’ chart faster than a manual diff result, leading to faster treatment. To report bands, a manual differential must be done. We must wait for a slide to be made, dry, and a diff to be analyzed either under the microscope or on CellaVision. Bands are subjective, relying on technologist interpretation.
So, why are we suddenly being asked to make bandemia a critical value?
Physicians asked for this change and have cited cases where patients were seen in the emergency department (ED) and subsequently released, later to return, or experiencing negative outcomes. These patients had bands reported on differentials. Other area hospitals are reporting bands and have critical values for bandemia. Because patients often are seen at more than one area hospital, and doctors may have privileges at more than one of these, for consistency, this makes sense. But is also makes sense clinically.
Recent data has drawn renewed attention to bands as a reliable predictor of severity of patient condition. A number of research papers have been published that indicate that bands may indeed be important for patient care. A 2012 study investigated bandemia in patients with normal white blood cell counts. This cohort study found that patients with normal WBC counts with moderate (11%-18%) or high (>20%) band counts had increased odds of having positive blood cultures and in-hospital mortality. (Drees, 2012)
In 2019 a study showed that there was an “increasing risk for death with increasing bandemia, irrespective of leukocyte count. (Davis, 2019) A 2021 study done at Rhode Island Hospital showed a strong correlation between increasing percentages of bands on an initial emergency room CBC and the likelihood of significant positive blood cultures and in-hospital mortality. This was noted even at band levels below 10%. (Hseuh, 2021) S. Davis, MD, from the Department of Emergency Medicine, George Washington University School of Medicine and Health Sciences, in Washington, DC wrote that “While emergency physicians may find reassurance in a normal leukocyte count, the balance of evidence strongly suggests a more prudent approach would be to wait for the bands.” (S. Davis, 2021) In other words, wait for that manual differential. He stated that emergency room physicians get results from automated CBCs before the manual diff and do not see or are aware of any internal laboratory flags on these specimens. Physicians should be aware of reporting processes to avoid early discharge of otherwise well-appearing patients before band counts are reported. Last year, trends in bandemia and clinical trajectory among patients was reviewed in a retrospective chart review at George Washington University Hospital. They noted that “Bandemia clearance and trending, in conjunction with other existing clinical tools, may be of use as a marker of improvement in sepsis. Conversely, worsening bandemia may be predictive of a deteriorating clinical status and possibly a higher mortality.” They also noted that following trends of band levels in patients with sepsis or septic shock may help to predict a clinical course and overall prognosis. (Prasanna, 2022) Additionally, a band count greater than 10% is one of the American College of Chest Physicians/Society of Critical Care Medicine’s systemic inflammatory response syndrome (SIRS) criteria used to diagnose sepsis. (Chakraborty, 2022) These are just a few of the many articles that support a clinical utility of reporting the band count.
When we first learned that we would be reporting bandemia as a critical value, we realized that we would need to get everyone on the same page. We do most of our diffs on CellaVision, so, in theory, that should be easy, but, and a big but, is that bands are notoriously subjective. Different technologists may have been taught or have used their own definitions of bands. Variation can occur depending on slide quality, tech training, definition of bands used, and number of cells counted. So, how do we make this work? We need to be sure that all our technologists are reporting bands using the same criteria, so we are not reporting differing or confusing information to physicians. The concern lies in a physician making a significant clinical decision based on apparent changes in band counts that are not real but only reflect predictable statistical factors and unpredictable technologist variability.
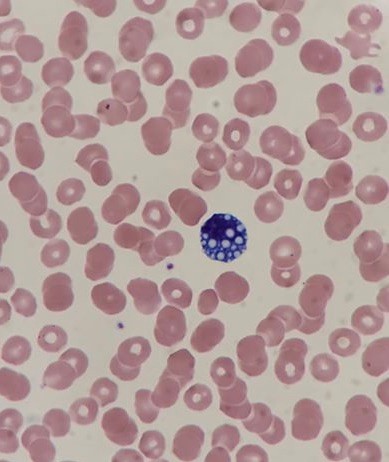
In our laboratory, we approached the implementation of this new critical value as an educational opportunity. Differentials that had been performed on our CellaVision were reviewed, and it was apparent that bands were not being categorized consistently among techs. (See Figure1) We started with reviewing the definition of bands with all technologists and writing updated detailed procedures that includes these definitions. We use CAP’s definition of bands, which is the definition used in most textbooks and references for over 60 years. (See Table 1) Many examples of both bands and segmented neutrophils were added to our reference library on CellaVision. These included textbook perfect bands and some that may be more subjective. These reference cells can be used by techs to compare cells when making decisions as to in which category they belong. It was also stressed to techs that they need to look at cells carefully, and in a view that is large enough to see both detail and differentiation.



Patient samples that had bands reported were located on CellaVision and multiple slides were made from these samples to be used as competency slides. In developing the differential evaluation tool, Rumke’s data showed that for a differential with a reported 12% bands, a second differential would have to have greater than 23% bands or fewer than 3% bands before the difference could be considered statistically significant. But this can be significant to our patients and patient care. In this example, diffs with <10% bands would not indicate bandemia, and diffs over 10% would initiate a critical bandemia call. And this could happen on the same slide depending on who did the diff, or on sequential samples on the same patient over a short period of time. These competency slides were assigned to techs to collect statistics on the mean and SD of the bands reported on each slide. Retraining and coaching will be provided as necessary. Follow up competency slides will be assigned, and statistics will be recalculated. The goal is to decrease variability in our band counts and to show that we have done so. This ongoing quality project has involved writing procedures, offering continuing education, assigning and reviewing competency slides, coaching technologists and reviewing slides with them and calculating statistics. Our goal is consistency and reporting meaningful results to our physicians.
As we saw in the studies cited above, % bands and trends are both important when evaluating clinical correlations. The chart below shows examples of how this might affect patient care. If a patient on presenting at the ED had a 19% band count, this would be called as a critical, and the patient would be further evaluated, and depending on clinical symptoms and medical history would likely have blood cultures drawn and be admitted to the hospital. If a second tech did the diff and reported 5% bands, the patient may be sent home without further evaluation. On subsequent CBCs, we could be giving confusing results to the physician if we are not consistent in our reporting. With multiple techs doing differentials on different shifts, it could look like this patient is getting better,
getting worse, or it could look like the patient is responding to therapy, and then the next day they had a setback. While we understand that bands will probably always be somewhat subjective, we need to narrow this down. By adhering to one definition, our goal is to report consistent and accurate results.

ED physicians are looking for an early marker that can be used to identify septic patients as early as possible. Bandemia may be used as this marker. We therefore need to be as objective as possible when reporting bands. “Ultimately the band count is only one factor amongst several others which will be used in assessing the patient’s clinical state and in determining any subsequent medical management. Yet, identifying bands is important, and emphasizes the key role that our laboratory professionals play in identifying causes for concern” Dr Edgar Alonsozana, Mercy Medical Center, Baltimore, Md.
I welcome your comments about how your laboratories report bands and if bandemia is a critical value in your facilities!
References
P.Joanne Combleet, Clinical utility of the band count, Clinics in Laboratory Medicine, 2002;22:101-136
Al-Gwaiz, Layla A. and H H Babay. “The Diagnostic Value of Absolute Neutrophil Count, Band Count and Morphologic Changes of Neutrophils in Predicting Bacterial Infections.” Medical Principles and Practice 16 (2007)
S. Davis, R. Shesser, K. Authelet, A. Pourmand. “Bandemia” without leukocytosis: A potential Emergency Department diagnostic pitfall. The American Journal of Emergency Medicine,Volume 37, Issue 10, 2019
Harada T, Harada Y, Morinaga K, Hirosawa T, Shimizu T. Bandemia as an Early Predictive Marker of Bacteremia: A Retrospective Cohort Study. Int J Environ Res Public Health. 2022 Feb 17;19(4):2275.
Christine DeFranco DO and Terrance McGovern DO MPH
St. Joseph’s Regional Medical Center, Paterson, NJ. Isolated Bandemia: What Should We Do with It? Critical Care, Oct. 2016,
Harmening, Denise. Clinical hematology and Fundamentals of Hemostasis, 4th ed. 1997
Prasanna N, DelPrete B, Ho G, et al. The utility of bandemia in prognostication and prediction of mortality in sepsis. Journal of the Intensive Care Society. 2022;0(0).
https://www.mlo-online.com/home/article/13007276/answering-your-questions
Takayuki Honda, Takeshi Uehara, Go Matsumoto, Shinpei Arai, Mitsutoshi Sugano, Neutrophil left shift and white blood cell count as markers of bacterial infection,Clinica Chimica Acta, Volume 457, 2016
Drees M, Kanapathippillai N, Zubrow MT. Bandemia with normal white blood cell counts associated with infection. Am J Med. 2012 Nov;125(11):1124.e9-1124.e15.
Leon Hsueh, Janine Molino, Leonard Mermel,
Elevated bands as a predictor of bloodstream infection and in-hospital mortality,The American Journal of Emergency Medicine,2021
https://www.ncbi.nlm.nih.gov/books/NBK547669/

-Becky Socha, MS, MLS(ASCP)CMBBCM graduated from Merrimack College in N. Andover, Massachusetts with a BS in Medical Technology and completed her MS in Clinical Laboratory Sciences at the University of Massachusetts, Lowell. She has worked as a Medical Technologist for over 40 years and has taught as an adjunct faculty member at Merrimack College, UMass Lowell and Stevenson University for over 20 years. She has worked in all areas of the clinical laboratory, but has a special interest in Hematology and Blood Banking. She currently works at Mercy Medical Center in Baltimore, Md. When she’s not busy being a mad scientist, she can be found outside riding her bicycle.