Hello! If you’ve been following my posts these last few months you’ve seen my work here in the country of Sint Maarten regarding the Zika virus outbreak. I have been very fortunate to be involved at various levels of work with this new epidemic from lab testing and seroprevalence research to public health and policy initiatives. As 2016 comes to a close, I would like to celebrate that work by highlighting a few great milestones here and offer a few thoughts for the future starting next year.
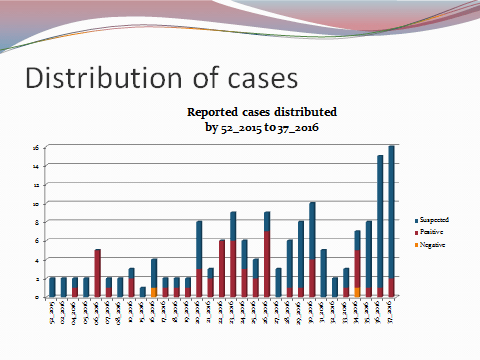
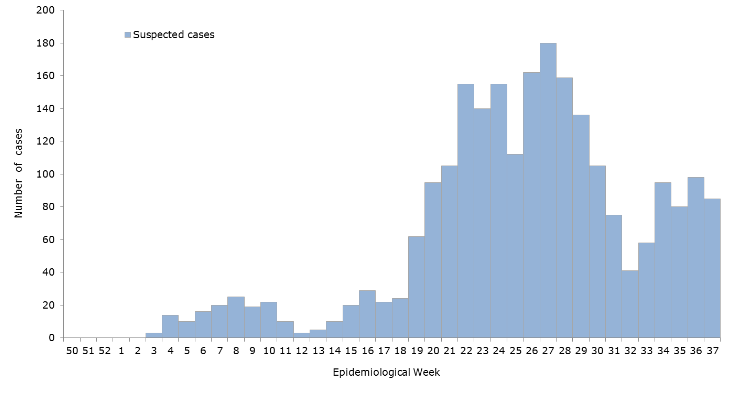
I mentioned before that immunological lab testing has been ongoing, targeting IgM and IgG seroprevalence of Zika virus (along with other Arboviruses i.e. West Nile, Chikungunya, Dengue, and Yellow Fever etc) within the community around my medical school. Nearly two hundred samples later—and counting—the results point to a presence of nearly 10-15% of people are confirmed positive for an active (IgM) or resolved (IgG) infection with Zika. Despite the small sample size and ever-developing data sets, these numbers are highly suggestive of a correlation mimicking that presented to us by the Ministry of Health (see my Zika virus primer post from October of this year). This holds promise for future studies like these which depend heavily on that type of medical laboratory science and analytics. My involvement in the seroprevalence project has been very rewarding and I have been able to contribute my experience and skills as a laboratory professional in writing SOPs/protocols, ensuring proper laboratory safety, and highlighting specimen collection standards. With several years as a medical laboratory scientist, I have been lucky to find a place to do such good work. The opportunity to step up as a leader when it comes to laboratory skills is always fulfilling!

Figure 1: Seroprevalence research and testing publicity for the AUC campus community, collection and specimen processing. photo credit: A. Yancone, 2016.
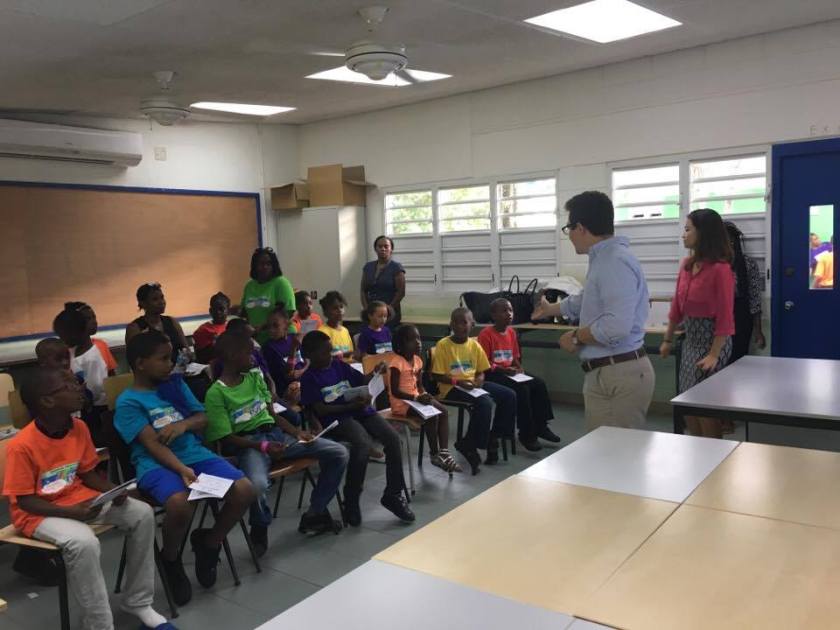
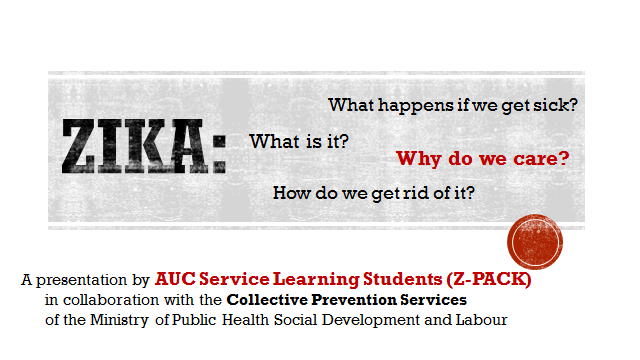
Along with the success of the lab-driven research at school, the project I spend the most time with is aimed at public health. My last post highlighted some of the successes my team and I have had with creating and maintaining a good relationship between members of the local Ministry of Health and the school system. In February earlier this year, my school strengthened their partnership with the Ministry by establishing a mission of public health initiatives driven by students and faculty who were engaged in community affairs, service learning, and public health. This increased sustainability will surely create a more long-lived effort for translational research to have an impact on health. I couldn’t be prouder of the work my team has done to show the community that medical students here represent the very best ASCP qualities of advocacy, partnership, and outreach through science and education. It is an honor to have my contributions recognized by the local public health officials—even moreso when they have now incorporated and sponsored my teams’ message of vector control and source reduction to schools across the island. Having children aged 4-16 enthusiastically repeat back to us and representatives from the Ministry they would “throw standing water away!” made a strong impact on public health officials, students, and their parents/families. Setting goals for the community’s health metrics are supported by local epidemiologic data and pushed forward by policy initiatives, and always rooted in diagnostics and laboratory-confirmed cases. This means that all of our efforts, all of my presentations, and each step along the way holds a foundation in laboratory science and continues to motivate me as we continue forward. We all know the lab-week tag line that “nearly 70% of a patient’s chart is lab-data-driven,” and I can attest that for issues in public health and policy the same if not more applies!

Figure 2: American University School of Medicine Partners with Sint Maarten Ministry of Health, Social Development, and Labour to bolster public health efforts and community involvement. AUC 2016.
Last month, Sint Maarten’s Ministry of Health sent Dr. Virginia Asin, the section director of the Collective Prevention Services office, to a Global Health Security Meeting in Miami. In this meeting she presented the policy initiatives her country had in dealing with risk reduction in the Caribbean. As a leader in this field, she cited ongoing partnerships with NGOs, public health offices, and medical professionals. She also shared her strong support for a project she said was truly a foundation for success—my team’s public health outreach! Dr. Asin and other staff members from the Ministry were present at an end-of-the-quarter presentation and meeting regarding this community outreach work based from the school. She shared with us her thoughtful admiration and ongoing support for the work we do here and said she was proud to have us as colleagues. Strong words and poignant sentiment from a real public health physician working in the field. It is incredible to have these efforts noticed by the Global Health Security Agenda (GHSA)! The GHSA exists at the forefront of the CDCs efforts to address the spread of various diseases, the global preparedness for them, and their economic impact on the global community. Dr. Asin and the Ministry’s continued support continue to inspire me, as well as other students, to look toward the future in creating more opportunities to merge medicine, data analytics, and positive outcomes.

Figure 3: Global Health Security Agenda platforms. GHSA and the CDC 2016.
Slated to begin in January of next year, my team will begin conducting a new project aimed at improving local health literacy and source reduction. Under our IRB proposals, we hope to gather the data about the residents of this island and subsequently match them with correlated health statistics (i.e. confirmed/reported Zika cases) and actively engage with the Ministry in improving these numbers. With this current momentum, I would argue that even though a few successful highlights have come, the best is yet to come. If I have learned anything during my time as a medical laboratory scientist, there is a certain exciting progress to the dynamic way data is being used as we move forward. Breakthroughs in communication and analysis are allowing these advancements to take off: ASCP pathologists consulting on cases of chronic diseases in Africa, growing credibility surrounds our profession as our voice accomplishes great things in Washington, and advancing diagnostics are getting more efficient every day. Hopefully, projects like the ones I keep all of you updated on will continue to strengthen the connections between the labs, media, and public health officials as we continue to improve outcomes globally.
Until next time! Happy Holidays and Have a Happy New Year!
(…and don’t keep standing water around if you live in a warmer area, because…vector control!)

-Constantine E. Kanakis MSc, MLS (ASCP)CM graduated from Loyola University Chicago with a BS in Molecular Biology and Bioethics and then Rush University with an MS in Medical Laboratory Science. He is currently a medical student at the American University of the Caribbean and actively involved with local public health.