Case 1 History
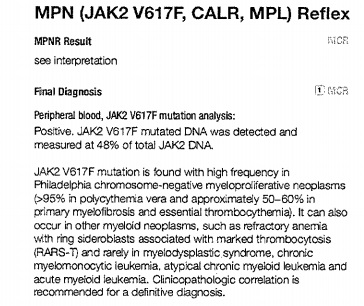
Sixty-one year old man with new diagnosis of Bud-Chiari syndrome and extensive peripheral, splenic and hepatic venous thrombosis with increasing fatigue, abdominal discomfort and abnormal liver function tests. A liver biopsy was performed and a hypercoagulability work-up, including JAK2 mutation analysis was initiated.

Diagnosis
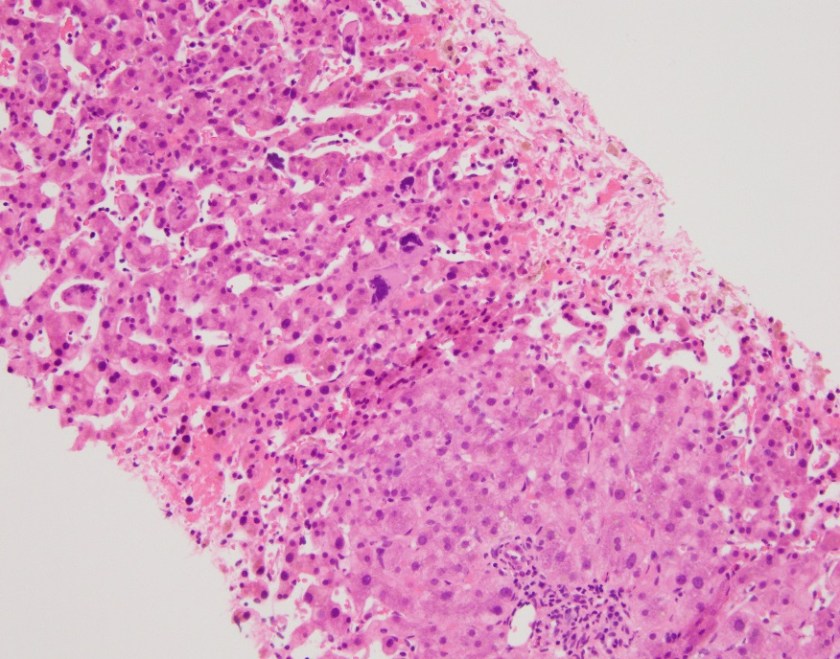
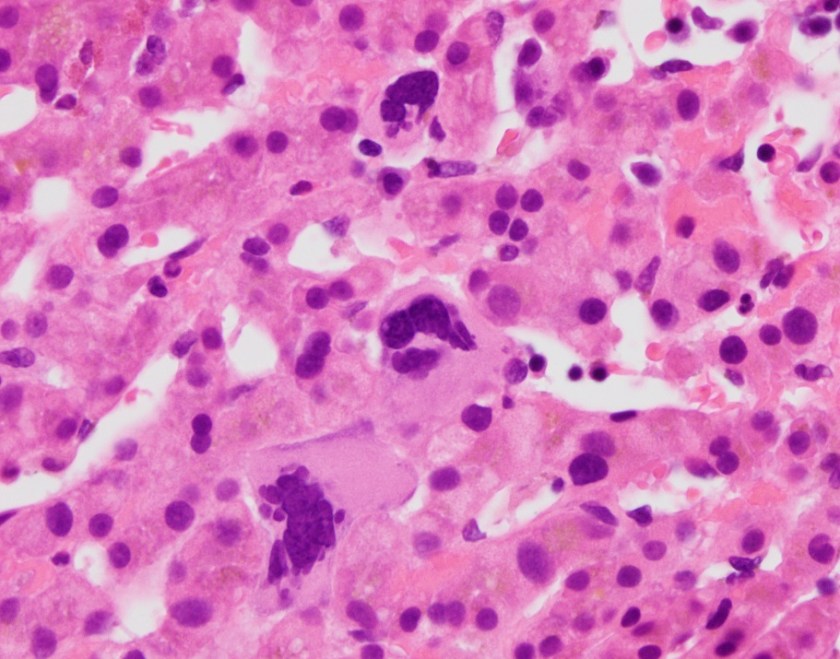
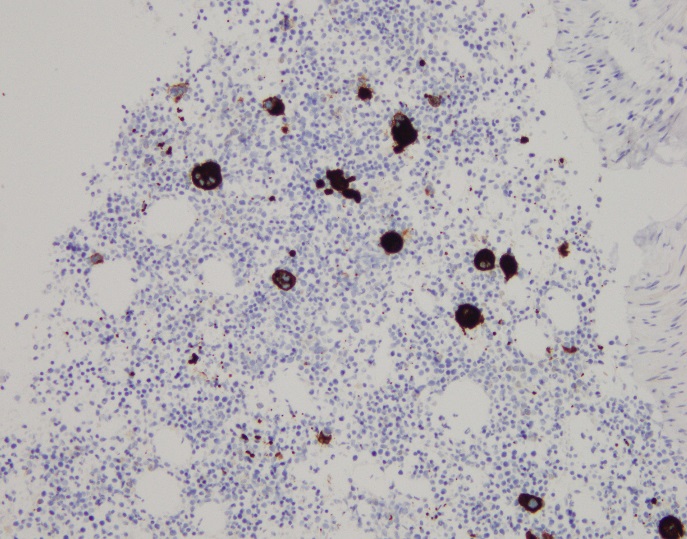
The liver biopsy showed extensive hemorrhage, hepatocellular necrosis and collapse with mild portal and lobular mixed inflammation. Occasional megakaryocytes and nucleated red blood cell precursors were noted. The case was sent to hematopathology for further review.

Hematopathology Diagnosis
Sections show liver parenchyma with changes of the patient’s known history of venous outflow obstruction, as well as extramedullary hematopoiesis, including scattered megakaryocytes (arrows) and erythroid precursors (circle). In the setting of a positive JAK2 V617F mutation, this constellation of findings is consistent with a myeloproliferative neoplasm.
Case 2 History
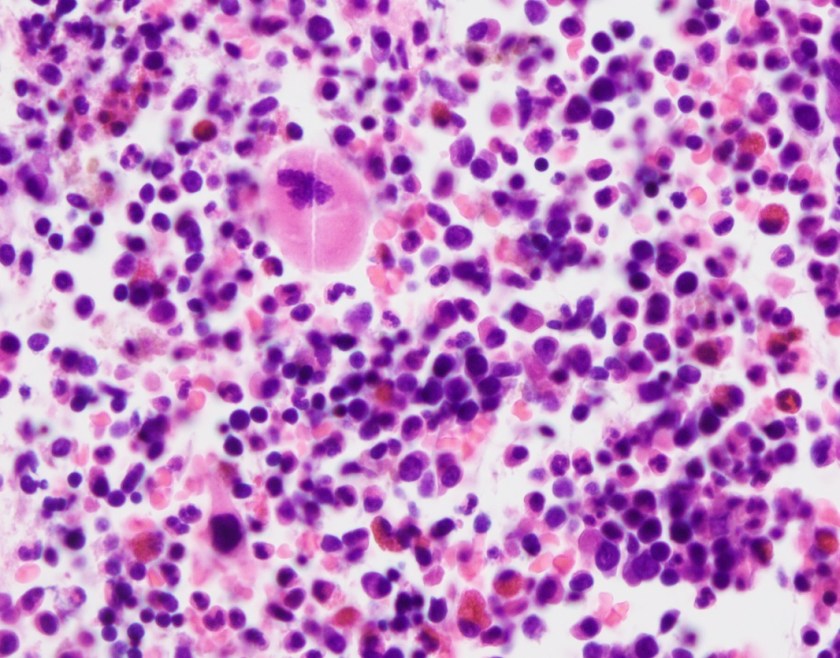
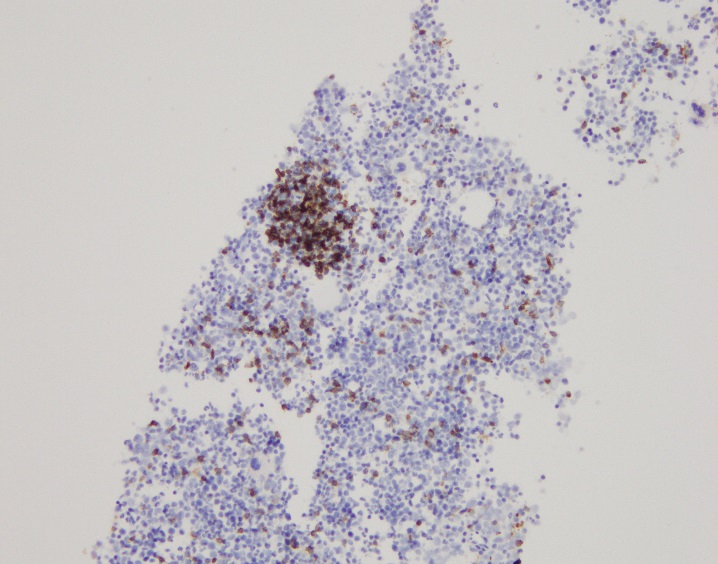
Fifty-nine year old man with a history of hypertension and alcohol abuse with posterior mediastinal lymphadenopathy. Recent bone marrow biopsy showed mildly hypercellular bone marrow with megakaryocytic and myeloid hyperplasia, and increased stromal reticulin with concern for primary myelofibrosis. A lymph node biopsy was performed.





Diagnosis
The lymph node biopsy shows fragments composed of adipocytes and maturing trilineage hematopoiesis. Multiple small to medium sized lymphoid aggregates are also seen, composed of small and mature appearing lymphocytes. The lymphocytes are a mixture of CD3 positive T cells and CD20 positive B cells with focal B cell predominance. Myeloperoxidase highlights myeloid precursors, which comprise 70-80% of the cellularity. CD71 highlights erythroid precursors, which comprise 20-30% of the cellularity. CD61 highlights megakaryocytes. CD34 highlights vessels and only rare CD34-positive cells are seen. Taken together, the findings are consistent with extramedullary hematopoiesis.
Discussion
Extramedullary hematopoiesis (EMH) is defined as hematopoiesis that occurs outside of the bone marrow. It can occur in both normal and pathologic states and has been seen in several hematologic disorders including chronic myeloproliferative neoplasms. Myeloproliferative neoplasms (MPN) are a group of clonal hematopoetic stem cell disorders that include polycythemia vera (PV), essential thrombocythemia (ET) and primary myelofibrosis (PMF).1 JAK2V617F mutation is the most frequent mutation associated with MPNs, found in roughly 96% of patients with PV and 65% of patients with ET and PMF. This mutation leads to constitutive activation of the JAK/STAT pathway and is a driver of myeloproliferation.2 The patient in case 1 was found to have a JAK2 mutation during the work-up for hypercoagulability. This suggests that he may have an underlying MPN, however JAK2 mutations have been found in patients with venous thrombosis, but without overt evidence of MPNs.3 The patient in case 2 had a bone marrow biopsy with features concerning for primary myelofibrosis. In PMF, there is generally a proliferation of myeloid cells in addition to marrow fibrosis. Increasing fibrosis can eventually result in pancytopenia as the fibrosis takes over the marrow space in addition to altering the bone marrow environment so that it is unable to support normal hematopoiesis. Ultimately, this can lead to extramedullary hematopoesis. EMH most commonly occurs in the spleen and liver, but has been described in many other sites including the mediastinum and lymph nodes. In addition to being a driver of proliferation, it is thought that JAK2 mutations make hematopoetic stem and progenitor cells more sensitive to growth factors and can cause the cells to mobilize to the liver and spleen.4 Patients with EMH can have symptoms related to the site of involvement. Depending on the extent of involvement and location, EMH may require treatment with low dose radiation. While EMH is a rare finding, it should prompt an investigation for an underlying MPN.
References
- Imai K, Aoi T, Kitai H,et al. A case of perirenal extramedullary hematopoiesis in a patient with primary myelofibrosis. CEN Case Reports. 2017;6(2):194-199. doi:10.1007/s13730-017-0274-1.
- Kim CH. Homeostatic and pathogenic extramedullary hematopoiesis. Journal of blood medicine. 2010;1:13-19.3https://www.ncbi.nlm.nih.gov/pubmed/17263783.
- De Stefano, V, Fiorini, A, Rossi, E, et al. Incidence of JAK2 V617F mutation among patients with splanchnic or cerebral venous thrombosis and without overt chronic myeloproliferative disorders. Journal of Thrombosis and Haemostasis. 2007;5(4):708-14. https://www.ncbi.nlm.nih.gov/pubmed/17263783.
- Passamonti F, Maffioli M, Caramazza D, et al. Myeloproliferative neoplasms: From JAK2 mutations discovery to JAK2 inhibitor therapies. Oncotarget. 2011;2(6):485-490.

–Chelsea Marcus, MD is a third year resident in anatomic and clinical pathology at Beth Israel Deaconess Medical Center in Boston, MA and will be starting her fellowship in Hematopathology at BIDMC in July. She has a particular interest in High-grade B-Cell lymphomas and the genetic alterations of these lymphomas.
