When it comes to laboratory testing at autopsy, our options are limited compared to those for living patients. We’ve previously discussed the complexities of postmortem toxicology testing (https://labmedicineblog.com/2023/05/23/toxicology-and-forensic-pathology-more-than-a-numbers-game/) but even basic laboratory studies like a glucose or sodium level cannot be reliably measured from postmortem serum specimens. Upon death, hemolysis and cellular breakdown rapidly set in; as tissue oxygen stores and ATP are depleted, the careful balance of intracellular and extracellular electrolytes is lost, making serum essentially useless as an analyte. This makes potentially lethal conditions which leave only non-specific clues (like diabetic ketoacidosis, dehydration, or hyponatremia) difficult or impossible to prove postmortem. Fortunately at autopsy we can access a unique, relatively protected body fluid which cannot be obtained from living patients- the vitreous humor.
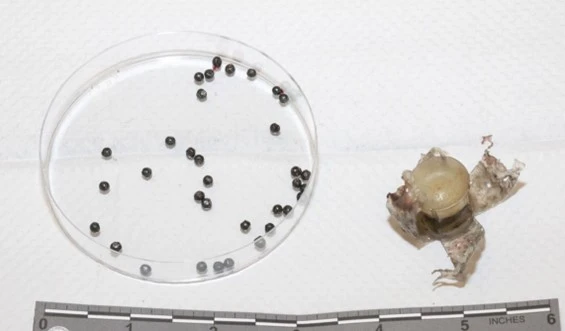
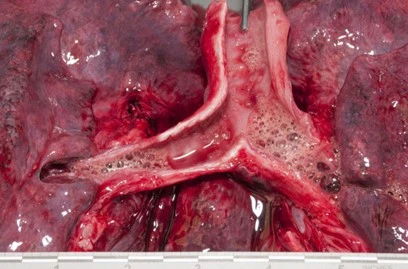
Vitreous humor is the clear, thick fluid which fills the globe of the eye. It is nearly acellular, composed predominantly of water with admixed hyaluronic acid and collagen proteins, and its insulated location provides it relative protection from the effects of decomposition and hemolysis. Vitreous humor is typically collected it at the beginning of an autopsy by inserting a needle into the most lateral aspect of the eye and aspirating the fluid; using this method, one can avoid collecting bits of retina (which interfere with analysis of the sample), and avoid creating any noticeable puncture marks or hemorrhages.
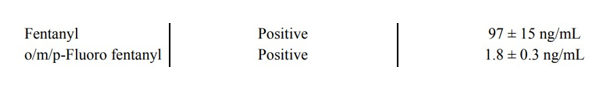
Years of data have shown that vitreous fluid approximates serum levels of major electrolytes, glucose, urea nitrogen (VUN), creatinine, ketones, and ethanol. Vitreous fluid is also valuable in the detection of 6-monoacetylmorphine (6-MAM), a metabolite of heroin which is quickly metabolized to morphine in the blood. Identifying 6-MAM in vitreous fluid allows us to ascertain a decedent used heroin, rather than just morphine.
While vitreous fluid is less affected by decomposition, it is not completely immune. The changes are predictable, though, and learning these patterns prevents misinterpretation of decomposition changes, and allows the pathologist to identify which results are still meaningful.
Vitreous fluid potassium will increase with the postmortem interval – in fact, this electrolyte is often touted (erroneously) as a method to determine time of death. Unfortunately there are many other variables (for example, antemortem potassium levels and rate of decomposition) affecting the rise of vitreous potassium, and this method has not proven to be the “holy grail” many were hoping for.
In contrast, vitreous sodium, chloride, and glucose levels all decrease following death – so while a low level may just be an artifact, a high level can be very meaningful. Even “low” levels should be assessed in the clinical context of the case and the concomitant potassium level. If the potassium is normal or barely elevated, it’s unlikely a “low” value is just decomposition-related.
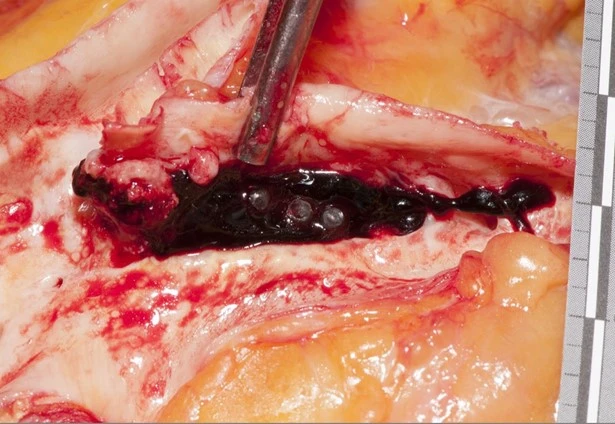
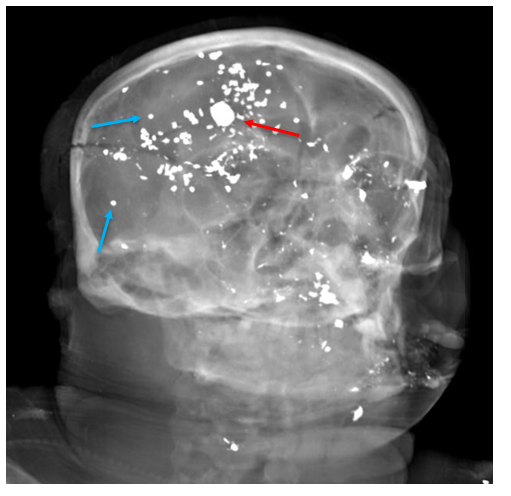
Vitreous humor poses some challenges in the laboratory, though. Because of the thick, viscous nature of the fluid, it can be challenging to actually run it through the instrument. As decomposition progresses, the eyes can desiccate and make the vitreous humor even thicker. In cases of eye trauma, intraocular hemorrhage can contaminate the vitreous humor as well. Importantly, in situations of suspected head trauma in infants, the recovery of vitreous fluid is deferred until the end of the autopsy. Retinal and optic nerve hemorrhages are usually not identified until the brain is removed, and we need to be sure that any trauma we identify was not created artificially during the autopsy.
In summary, the use of vitreous humor as an analyte is a great illustration of creative problem solving. At autopsy the quality of blood specimens is limited, but we aren’t limited to blood. This lesson can be translated to any area of the laboratory: thinking outside of the proverbial box can lead to unexpected, paradigm-shifting opportunities.
References
Rose KL, Collins KA. Vitreous postmortem chemical analysis. NewsPath. December 2008.
Wyman J, Bultman S. Postmortem distribution of heroin metabolites in femoral blood, liver, cerebrospinal fluid, and vitreous humor. J Anal Toxicol. 2004 May-Jun;28(4):260-3. doi: 10.1093/jat/28.4.260. PMID: 15189677.

-Alison Krywanczyk, MD, FASCP, is currently a Deputy Medical Examiner at the Cuyahoga County Medical Examiner’s Office.