Case History
A 49 year old African American female was transferred from an outside hospital due to orbital cellulitis. Her past medical history was significant for HIV, CNS lymphoma, for which she was taking methotrexate & rituximab, and type II diabetes. Her vitals were: blood pressure 181/145, heart rate 145, temperature 98.6°F and respiratory rate 20. On physical examination, her right eye was bulging, with conjunctiva & eyelid swelling, and her iris was non-reactive. Scant serous drainage was noted. Admission labs showed a normal white blood cell count (9.8 TH/cm2), glucose of 211 mg/dL (normal: 74-106 mg/dL), hemoglobin A1C of 7.7% (normal: 4.2-6.0%) and platelets were low at 41,000 TH/cm2. An infection was suspected and the patient was started on vancomycin and piperacillin-tazobactam. She had a head CT scan which showed right periorbital cellulitis and diffuse sinus disease but no abscess formation. Nasal endoscopy was performed and extensive adhesions & black colored, necrotic tissue of the right nasal cavity was noted in addition to whitish debris, consistent with fungal overgrowth extending into the nasopharynx. Biopsies were taken for frozen section and bacterial & fungal culture and Infectious Disease was consulted for management of a probable rhinocerebral fungal infection.
Laboratory Identification


Discussion
Rhizopus spp. belong to the order Mucorales, are ubiquitous in the environment and are the most common etiologic agents of mucormycosis. Rhizopus spp. typically cause invasive infections in the nasal sinus, brain, eye and lung, particularly in patients that have uncontrolled diabetes, HIV or are immunosuppressed. Mucorales are angioinvasive, exhibit perineural invasion and there is usually thrombosis, infraction and necrosis of surrounding tissue. As the illness can progress quite rapidly, prompt diagnosis and treatment is necessary.
If a Mucorales is suspected, tissue specimens obtained during a surgical procedure should be sent for frozen section, direct examination with calcofluor white/KOH and fungal culture. On histologic exam or microscopic exam in the microbiology laboratory, the hyphae of Rhizopus spp. are wide & ribbion-like with few to no septations (pauci- or aseptate) and wide angle branching (90°) (Image 1). Further classification requires culture.
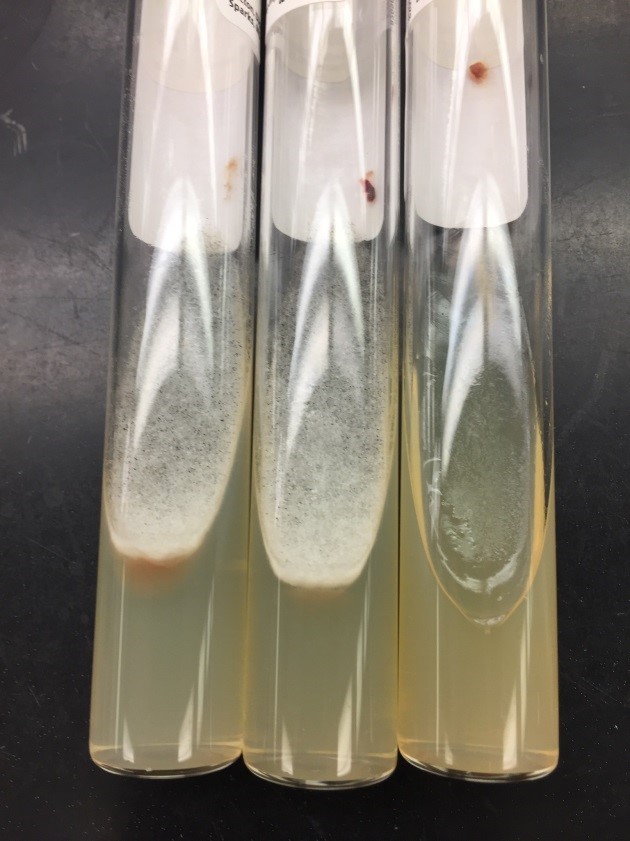
If a Mucorales is suspected, the tissue submitted for fungal culture should be minced into small pieces and directly applied to the appropriate fungal media. Grinding of tissue will kill the hyphae and result in no growth from culture. Mucorales will not grow on media containing cycloheximide. Rhizopus spp. grow rapidly within 1-4 days and start as white, fluffy colonies that become grey or brown in color as they mature (Image 2). The Mucorales are described as “lid lifters” due to their rapid growth and “cotton candy” like colonies that fill the plate. On lactophenol cotton blue prep, Rhizopus spp. have unbranching sporangiophores that terminate in a round sporangium and arise directly under well-developed rhizoids (Image 3). The sporangium ruptures when mature and releases many oval sporangiospores.
Treatment of patients with mucormycosis is usually a dual approach with wide surgical excision and amphotericin B, which has been shown to be an effective anti-fungal drug in the majority of Mucorales. In contrast, voriconazole has poor activity against these isolates. If susceptibility testing is needed, CLSI provides reference broth microdilution guidelines. In the case of our patient, due to the grave prognosis of her condition, in addition to her other comorbidities, the family elected for comfort care measures only and board spectrum anti-fungals were not started.

-Lisa Stempak, MD, is an Assistant Professor of Pathology at the University of Mississippi Medical Center in Jackson, MS. She is certified by the American Board of Pathology in Anatomic and Clinical Pathology as well as Medical Microbiology. She is the Director of Clinical Pathology as well as the Microbiology and Serology Laboratories. Her interests include infectious disease histology, process and quality improvement and resident education.
