Case History
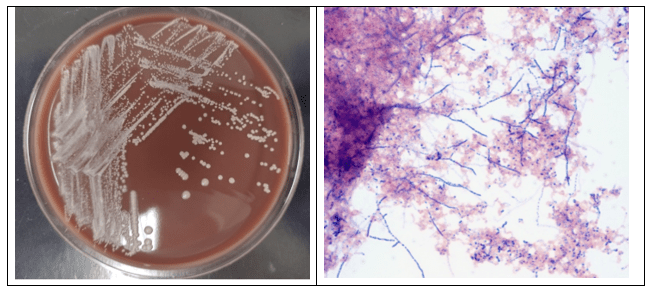
A 67 year old female presented to the emergency department with worsening chest pain and shortness of breath for several weeks. Her medical history was notable for diffuse large B cell lymphoma, for which she had started treatment with rituximab and tafastimab-cxix. Her complete blood count revealed severe leukopenia. A chest computed tomography scan showed focal consolidation in the right lower lobe, and broad-spectrum antibiotics and Filgrastim were started to treat her pneumonia. However, her symptoms did not improve. She underwent a bronchoalveolar lavage, which was sent to microbiology for culture. The initial Gram stain of the specimen was unrevealing. Twelve days later, a pathogen was isolated from cultures with acid-fast media and fungal media. On a Sheep’s blood agar plate, white, chalky colonies appeared. A Gram stain of the isolate showed gram-positive organisms growing as branching, beaded filaments. The organisms were further highlighted on a partial acid-fast stain. MALDI-TOF identified the organism as Nocardia farcinica. The patient was started on trimethoprim/sulfamethoxazole and imipenem, and was discharged following clinical improvement.
Discussion
Once mistakenly classified as a fungus due to its filamentous, branching morphology, Nocardia spp. are actually gram-positive, aerobic bacteria that belong to the order Cornybacteriales1. Nocardia are normal inhabitants of the soil, where they digest decaying plant matter. However, they are a cause of human disease in susceptible hosts when they are inhaled or enter via the skin2,3 . The major risk factor for infection is an immunocompromised state, particularly defects in cell-mediated immunity. As such, patients with AIDS or lymphoma, those receiving allogeneic organ transplants, and those taking immunosuppressive drugs including high-dose steroids either are more susceptible to infection or suffer more severe disease2,4. Among persons with intact immune defenses, underlying lung diseases such as chronic obstructive pulmonary disease or cystic fibrosis, predispose to infection1.
The most common clinical manifestation of Nocardiosis, particularly in immunocompromised hosts, is a subacute to chronic pneumonia that can wax and wane, and abscesses are a characteristic pathologic feature4. Nocardia can spread via the blood to affect virtually all other organs, with the brain, eyes, and joints being common sites of dissemination1,5,6. Skin infections, more common in immunocompetent persons, include cellulitis and a lymphocutaneous disease that mimics Sporotrichosis4,5. Specifically for Nocardia farcinica, this species have been shown to be involved in disseminated diseases, with most patients being immunocompromised, but in immunocompetent individuals, cutaneous infections have been reported.
Often the first diagnostic clue comes from visualization of gram-positive beaded, thin, branching organisms on direct smears of specimens7. Of note, while the beaded, branching morphology is characteristic, this appearance is sensitive to several culture conditions including media and temperature. Given that Nocardia does not stain fully on Gram stain, it is recommended that a modified acid-fast stain be done as a reflex stain to confirm the suspicions. Organisms, aside from true Mycobacteria, that contain mycolic acids on the cell wall include Nocardia, Gordonia, Dietzia, Rhodococcus, Segmiliparus, Tsukamurella, and Williamsia. However, in some cases, not all organisms can be seen on the direct smear, which warrants cultures to rule out infection but Nocardia spp. can be difficult to isolate in culture either due to low numbers in the initial specimen, or overgrowth by contaminating bacteria3. They grow slowly, usually over the course of weeks3,4. Nocardia can be isolated from most media used to culture bacteria, fungus and mycobacteria3,7. Colonies often appear white and dry but appearance of velvety, powdery, wrinkled, or being heaped are also not uncommon. On the reverse of the plate, the colors may vary and can be brown, tan, pink, orange, red, purple, gray, yellow, peach, or white. The partial acid-fastness of Nocardia spp. is an important corroborating piece of evidence7. Molecular and proteomic methods, including 16S rRNA sequencing and MALDI-TOF allow for definitive confirmation1,7.
A diagnosis of Nocardiosis aids in the selection of appropriate antibiotics and may raise suspicion for disseminated disease, such as brain abscesses. Trimethoprim/sulfamethoxazole remains the antibiotic of choice, and patients usually respond within weeks4. Adding another potent antibiotic such as imipenem helps treat more severe or disseminated disease6. Studies done in-vitro have shown that isolates with resistance to Trimethoprim/sulfamethoxazole are typically susceptible to carbapenems.
References
1. Traxler RM, Bell ME, Lasker B, Headd B, Shieh WJ, McQuiston JR. Updated review on Nocardia species: 2006-2021. Clin Microbiol Rev. 2022;35(4).
2. Steinbrink J, Leavens J, Kauffman CA, Miceli MH. Manifestations and outcomes of nocardia infections. Medicine (Baltimore). 2018;97(40).
3. Lerner PI. Nocardiosis. Clin Infect Dis. 1996;22(6):891-903.
4. Filice GA. Chapter 174: Nocardiosis. In: Harrison’s Principles of Internal Medicine. 21e ed. McGraw Hill; 2022. https://accessmedicine-mhmedical-com.proxygw.wrlc.org/content.aspx?bookid=3095§ionid=263964309
5. Mochon AB, Sussland D, Saubolle MA. Aerobic actinomycetes of clinical significance. Microbiiology Spectr. 2016;4(4).
6. Langoya CO, Henderson NM, Sutherland RK. Nocardia and Actinomyces. Medicine (Baltimore). 2021;49(12):756-759.
7. Tille PM. Chapter 18 Nocardia, Streptomyces, Rhodococcus and similar organisms. In: Bailey & Scott’s Diagnostic Microbiology. 15th ed. Elsevier; 2022.
-Stevephen Hung MD, PhD is currently a PGY-4 resident at George Washington University Hospital. He graduated from Case Western Reserve University School of Medicine in Cleveland, OH. His academic interests include transfusion medicine, informatics and molecular pathology.

-Rebecca Yee, PhD, D(ABMM), M(ASCP)CM is the Chief of Microbiology, Director of Clinical Microbiology and Molecular Microbiology Laboratory at the George Washington University Hospital. Her interests include bacteriology, antimicrobial resistance, and development of infectious disease diagnostics.

Hello, I am a MLT student currently, and this case is interesting. I’ve learned about Nocardia, but it is intriguing to see it in a rea life case.