Case description
A 72 year-old male with severe aortic stenosis resulting in heart failure underwent aortic valve replacement and became febrile with mild shortness of breath on post-operative day one. Additional pertinent medical history includes end-stage renal disease secondary to diabetic nephropathy with kidney transplantation seven months prior which was complicated by delayed graft function requiring hemodialysis and immunosuppression. The patient’s presentation was suspicious for either a post-operative fever or a complication of hemodialysis. Physical examination did not suggest infection at either the surgical site or his arteriovenous fistula. A chest CT revealed a moderate, loculated left pleural effusion with left lower lobe atelectasis and nodular consolidations in the right lung, raising concern for pneumonia. A bronchial biopsy was obtained, and histopathological evaluation was consistent with an abscess, but no organisms were visualized. Culture from a left bronchial brushing was also obtained at the same time. Two days later, the patient developed a progressively enlarging forehead lesion (Image 1).

Laboratory Identification
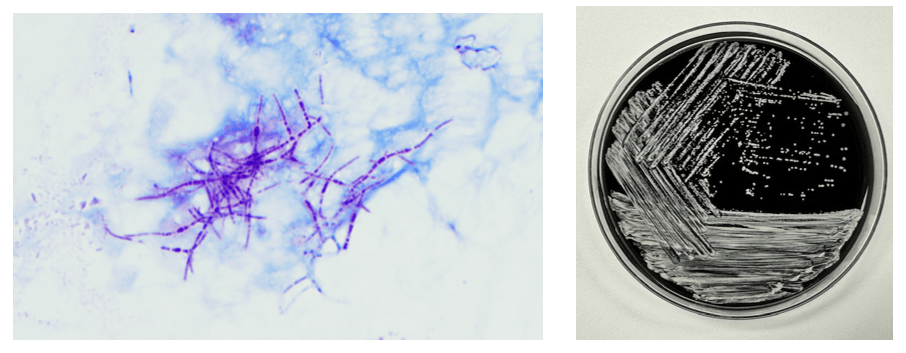
Microscopic evaluation of the biopsy of the lesion for culture revealed branching, beaded gram positive filamentous bacteria which stained positive using a modified acid-fast stain, suggestive of Nocardia species. This was corroborated by the bronchial culture, where similar modified acid-fast organisms were visualized and grew chalky white colonies identified as Nocardia sp. by MALDI-TOF MS (Image 2). The isolate was referred to a reference laboratory for definitive speciation and antimicrobial susceptibility testing, and the patient was started empirically on ceftriaxone and trimethoprim/sulfamethoxazole. Speciation and susceptibility testing subsequently identified the organism as Nocardia brasiliensis with susceptibility to both ceftriaxone and trimethoprim/sulfamethoxazole, and treatment was thereafter continued for 40 days.
Discussion
Nocardia is a saprophytic bacterium that is commonly found in soil worldwide. Gram staining of Nocardia sp. usually reveals delicate, weakly or erratically staining, beaded, branching Gram-positive rods. There are currently 130 known species of Nocardia,1 of which more than 50 have been reported to have clinical relevance.2 Disease due to Nocardia is known to occur due to inhalation of the organism from the environment or traumatic inoculation. It is thought to be an opportunistic pathogen most commonly affecting immunocompromised patients3 like the patient in this case.
Manifestations of nocardiosis vary widely depending on the species responsible, with most common presentations being lymphocutaneous, pulmonary, or disseminated disease. Here, we present a patient who displayed both lymphocutaneous and pulmonary forms of Nocardia infection. While prognosis is poorer in immunocompromised patients, with appropriate treatment, recovery rate is high in both lymphocutaneous and pulmonary forms, unlike in disseminated disease, where studies have found mortality rates between 44% to 85%.4
Diagnosis of Nocardia infections is mainly performed through either direct visualization of the organism or through culture. The modified acid-fast stain is commonly performed but has limited sensitivity and should generally be performed in conjunction with the Gram stain.5 Recovery in culture is most reliable from respiratory and/or tissue samples, while blood culture, by contrast, has poorer yield. While some strains, as in this patient, appear within several days in culture, some strains may take up to 2 to 3 weeks to detect5 necessitating extended incubation and consultation with the clinical laboratory.
Treatment requires prolonged courses of antibiotics. Susceptibilities vary by species, making it important to obtain species identification to identify appropriate therapy to guide empiric therapy. Susceptibility testing is performed to allow further tailoring of antibiotic regimens. In this case, the patient was treated with a combination of trimethoprim/sulfamethoxazole and ceftriaxone, both of which cover the majority of clinically relevant Nocardia species, until susceptibility testing revealed that the empiric treatment provided adequate coverage for the Nocardia brasiliensis identified, supporting continuation of the chosen empiric regimen.
References
- Genus Nocardia. List of Prokaryotic names with Standing in Nomenclature. https://www.bacterio.net/genus/nocardia (2023).
- Hamdi AM, Fida M, Deml SM, Abu Saleh OM, Wengenack NL. Retrospective Analysis of Antimicrobial Susceptibility Profiles of Nocardia Species from a Tertiary Hospital and Reference Laboratory, 2011 to 2017. Antimicrob Agents Chemother. 2020 Feb 21;64(3):e01868-19. doi:10.1128/AAC.01868-19.
- McNeil MM, Brown JM. The medically important aerobic actinomycetes: epidemiology and microbiology. Clin Microbiol Rev. 1994 Jul;7(3):357-417. doi:10.1128/CMR.7.3.357.
- Traxler RM, Bell ME, Lasker B, Headd B, Shieh WJ, McQuiston JR. Updated Review on Nocardia Species: 2006-2021. Clin Microbiol Rev. 2022 Dec 21;35(4):e0002721. doi: 10.1128/cmr.00027-21.
- Saubolle MA, Sussland D. Nocardiosis: review of clinical and laboratory experience. J Clin Microbiol. 2003 Oct;41(10):4497-501. doi: 10.1128/JCM.41.10.4497-4501.2003.
-Albert Budhipramono, MD, PhD, is currently a PGY1 Clinical Pathology Resident at the University of Texas Southwestern Medical Center in Dallas, Texas.

-Clare McCormick-Baw, MD, PhD is an Assistant Professor of Clinical Microbiology at UT Southwestern in Dallas, Texas. She has a passion for teaching about laboratory medicine in general and the best uses of the microbiology lab in particular.

-Andrew Clark, PhD, D(ABMM) is an Assistant Professor at UT Southwestern Medical Center in the Department of Pathology, and Associate Director of the Clements University Hospital microbiology laboratory. He completed a CPEP-accredited postdoctoral fellowship in Medical and Public Health Microbiology at National Institutes of Health, and is interested in antimicrobial susceptibility and anaerobe pathophysiology.

With that history (before the symptoms described), CMV was my first thought.