A 36 year old male was referred to gastroenterology after presenting to the emergency room for hematemesis and severe fatigue. He was pale and tachycardic, and the CBC showed a hemoglobin of 4.5. An esophagastroduodenoscopy (EGD) at the time demonstrated erosive esophagitis with a visible vessel and was treated with a PPI. A repeat scope the following month no longer demonstrated a vessel but identified a 10 cm ulcerative gastric cardia mass at the GE junction. Forcep biopsies showed a gastric ulcer with granulation tissue, and the stains performed yielded results that were not consistent with carcinoma or lymphoma; however, the biopsy material was limited, and the patient was referred to our GI clinic for further workup.
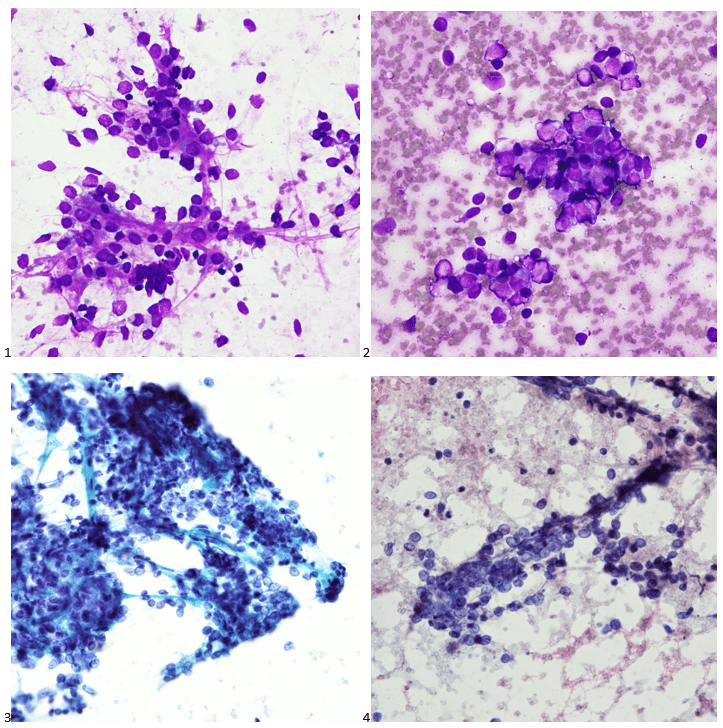
The interventional gastroenterologist requested cytology be present for the patient’s endoscopic ultrasound to ensure an adequate specimen was obtained for a definitive diagnosis. During the rapid onsite evaluation (ROSE), we determined the Diff-Quik smear was adequate, and the pathologist could confidently suggest that tumor cells were present. We collected additional FNA passes in our cell block tube to run ancillary studies.
The following morning, all we could make of the case was that it was a poorly-differentiated malignant neoplasm with spindle and epithelioid features. The cytoplasm was minimal and fairly wispy while the nuclei were hypochromatic and fragile with nuclear grooves and nucleoli. On the Diff-Quik smears, the cytoplasm looked blue, which pointed us in the direction of possibly lymphoma or neuroendocrine, but the clustering made me favor neuroendocrine. With the pap-stained smears, were torn between carcinoma and a neuroendocrine tumor, maybe even an epithelioid GIST, albeit an odd location. And of course, there’s always the differential of melanoma, the great mimicker. Off to IHC we go!
When our immunostains were delivered later that afternoon, our pathologist came up to me and said, “I got it! I know what it is!” Ecstatic, I replied, “What is it? Lymphoma? Carcinoma? GIST? MELANOMA?” “No, it’s a WEIRDOMA! Nothing is staining positive. No epithelial markers, no definitive lymphoid markers… nothing. It’s a weird case. I have to run additional stains.”
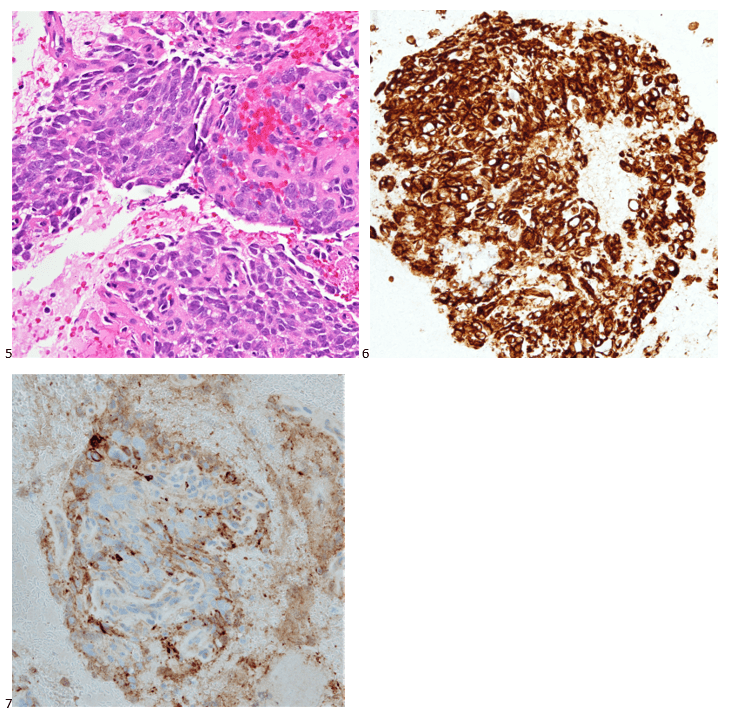
Back to the drawing board and 20 additional recut sections later, more immunostains were ordered and a mixed profile led us down a more confusing path. The tumor cells show positive staining for vimentin, CD56, and CD10 (focal), and negative staining for AE1/AE3, Cam5.2, CK7, desmin, SMA, HHF35, CD34, CD117, DOG-1, S100, SOX-10, synaptophysin, SALL4, CD45, CD68, and CD21. Proliferative index by Ki-67 was approximately 35%. The morphology and immunoprofile of the tumor were highly unusual, suggesting a mesenchymal neoplasm, possibly a sarcoma.
The concurrent forcep biopsies demonstrated rare atypical cells that were difficult to classify due to the limited number of cells, the non-specific morphology, and the following non-specific immunophenotype: positive staining for CD99, partial positive staining for D2-40 and NSE, and focal or weak positive staining for Cam5.2, while negative for AE1/AE3, CK7, EMA, S100, CD31, desmin, PAX8, BCL2, and myogen. The biopsy tissue consisted of predominantly ulcerative tissue and a fragment of squamous mucosa with a lamina propria infiltrate of atypical cells with spindle and epithelioid morphology.
Due to the FNA cell block consisting of 80% tumor compared to the limited forcep biopsy tissue, we sent FFPE cell block sections for RNA fusion studies to help us further classify the tumor. An EWSR1::ERG (in-frame) rsa(22;21)(q12.2;q22.2) gene fusion was detected in the tissue sample, which has been reported in extraskeletal Ewing sarcoma.
Stomach, GE Junction, EUS-FNA Final Diagnosis: Ewing Sarcoma
Fortunately, the patient’s PET scan did not demonstrate any evidence of metastatic disease, and the patient along with his care team decided to pursue systemic therapy as these tumors tend to be chemosensitive. The need for radiation therapy will be reviewed depending on the tumor’s response to systemic therapy. A strange presentation, this visceral Ewing sarcoma, and a reason why immunostains and molecular profiling are so important to rendering a definitive diagnosis. In our study set files, however, it will forever be dubbed my favorite weirdoma.

-Taryn Waraksa-Deutsch, MS, SCT(ASCP)CM, CT(IAC), has worked as a cytotechnologist at Fox Chase Cancer Center, in Philadelphia, Pennsylvania, since earning her master’s degree from Thomas Jefferson University in 2014. She is an ASCP board-certified Specialist in Cytotechnology with an additional certification by the International Academy of Cytology (IAC). She is also a 2020 ASCP 40 Under Forty Honoree.
