Case History
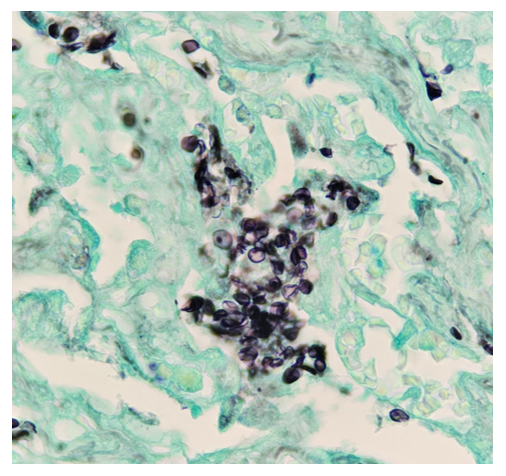
A 21-year-old male with no significant past medical history presented to the emergency department for acute hypoxemic respiratory failure. He also reported a productive cough with green sputum and unintentional 30 lb weight loss over the past 5 months. On presentation, his oxygen saturation was in the 80s on room air and initial labs were significant for lactic acidosis and a reactive HIV Ag/Ab. His HIV viral load was 1,359,029 copies/mL with a CD4 count of 37 cells/mm3 . Imaging included a chest X-ray and chest CT, which revealed left sided pneumothorax and diffuse ground glass opacities with scattered areas of consolidation. Based on his clinical presentation and CD4 counts <200 cells/mm3, the patient was started on trimethoprim/sulfamethoxazole (TMP/SMX) for PCP prophylaxis. A bronchoalveolar lavage was performed but had no growth on bacterial and fungal cultures. On hospital day 5, the left-sided pneumothorax was persistent despite multiple chest tube placements and a right-sided pneumothorax had formed, and the patient underwent video-assisted thoracoscopic surgery and pleurodesis. During the procedure, a ruptured bleb was found at the apex of the upper lobe of the left lung and a limited apical wedge resection was performed. Pathologic examination of the resection was significant for foamy exudate-filled alveoli on H&E staining. GMS stain revealed cup-shaped organisms confirming the presence of Pneumocystis jirovecii. The patient was continued on TMP/SMX for 21 days total and weaned off supplemental oxygen with follow-up scheduled at an HIV clinic.
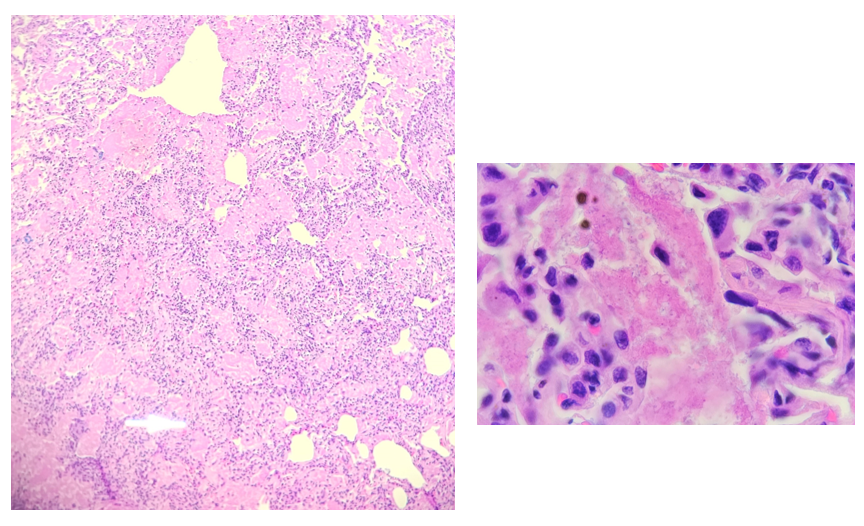
pink, foamy amorphous material (20x and 100x magnification)
Discussion
Pneumocystis jirovecii pneumonia (PCP pneumonia) is a life-threatening infection found in immunocompromised patients, with approximately a third of patients affected being HIV-positive.1 Although the incidence of infection in HIV-positive patients is declining with modern therapies, it is still commonly seen in undiagnosed HIV-positive patients who present late in the course of the disease.2
Clinically, PCP pneumonia is characterized by dyspnea, tachypnea, cough, and fever in an immunocompromised patient. Chest imaging features include bilateral interstitial infiltrates and a “ground glass” appearance on CT. Because Pneumocystis is extremely challenging to culture, diagnosis relies on these clinical findings with confirmation by staining or PCR testing of bronchoalveolar lavage fluid or lung biopsy.3 Stains that can be used to identify PCP pneumonia include Gromori-methenamine silver (GMS) stain, calcofluor white (CW) stain, Toluidine Blue O (TBO) stain, with GMS and CW stains having the highest sensitivity.3,4 On GMS stain, the cyst wall of Pneumocystis will appear black with a “crushed ping-pong ball” or crescent shaped appearance.
Treatment with TMP/SMX should be started in patients with suspected PCP pneumonia while work-up is pending. Corticosteroids can also be added to the treatment regimen in patients with more severe respiratory symptoms (5). After completion of 21 days of therapy, a lower-dose of TMP/SMX should be continued in HIV-positive patients with CD4+ counts less than 200 for prophylaxis.5
References
- Roux, Antoine, et al. “Pneumocystis Jirovecii Pneumonia in Patients with or without AIDS, France.” Emerging Infectious Diseases, vol. 20, no. 9, 2014, pp. 1490–1497, https://doi.org/10.3201/eid2009.131668.
- White, P. Lewis, et al. “Pneumocystis Jirovecii Pneumonia: Epidemiology, Clinical Manifestation and Diagnosis.” Current Fungal Infection Reports, vol. 13, no. 4, 2019, pp. 260–273, https://doi.org/10.1007/s12281-019-00349-3.
- Bateman, Marjorie, et al. “Diagnosing Pneumocystis Jirovecii Pneumonia: A Review of Current Methods and Novel Approaches.” Medical Mycology, vol. 58, no. 8, 2020, pp. 1015–1028, https://doi.org/10.1093/mmy/myaa024.
- Procop, G. W., et al. “Detection of Pneumocystis Jiroveci in Respiratory Specimens by Four Staining Methods.” Journal of Clinical Microbiology, vol. 42, no. 7, 2004, pp. 3333-3335, https://doi.org/10.1128/jcm.42.7.3333-3335.2004.
- Vilar, et al. “The Management of Pneumocystis Carinii Pneumonia.” British Journal of Clinical Pharmacology, vol. 47, no. 6, 1999, pp. 605–609, https://doi.org/10.1046/j.1365-2125.1999.00966.x.

-Alice Ann Lever is a fourth-year medical student at the Medical College of Georgia. She is interested in hematopathology and surgical pathology.
-Hasan Samra, MD, is the Director of Clinical Microbiology at Augusta University and an Assistant Professor at the Medical College of Georgia.
