In June 2024, BD (Becton Dickinson) notified their customers that there will be a global shortage of BACTEC blood culture bottles which is anticipated to last several months. Blood culture bottles are critical for diagnosing infections in patients, and their scarcity could lead to delays in diagnosis and challenges in managing patient care, especially for those with serious systemic infections. During supply shortages, it is paramount that management relies heavily on careful inventory oversight, and prudent use and stewardship of available reagents. Here we will summarize key measures recommended to ensure continuity of care. However, it must be emphasized that there is no ‘one size fits all’ approach and each institution need to consider what works best for their patients and workflow. It is a team effort-laboratorians must work collaboratively with infectious disease providers, hospital leadership, supply management teams and other stakeholders to implement and manage efforts without duplication of efforts.
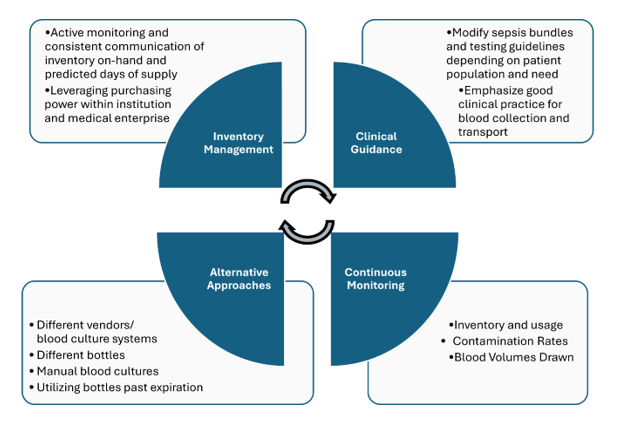
- Inventory Management:
- There needs to be continuous monitoring and communication among all stakeholders regarding inventory and usage. It is imperative that hospital leadership are aware of the current inventory on-hand and the predicted days of supply.
- If the hospital is within a medical center, consider centralizing supplies and reallocating to those in dire need. If your institution is part of a larger system or corporation, consider leveraging system’s purchasing power vs. a single institution purchasing power to ensure availability of the blood culture bottles.
- Clinical guidance:
- In many institutions, laboratory and infectious disease teams, in collaboration with the clinical partners, developed sepsis bundles, in which blood cultures and lactic acid testing are the corner stones of the bundle. Most of the time, such bundles are built around the CMS guidelines, as part of the overarching Medicare’s Hospital Value-Based Purchasing Program (VBP). Such bundles are great tools to promote the best standard of care practices, as well as serving as a standard communication tool. Most organizations institute two separate types of sepsis bundles: the severe sepsis bundle and the sepsis shock bundle. With time, we need to consistently leverage quality and patient safety approaches, as well as regulatory standards to ensure the most optimal test utilization overall, especially during the times of shortages. Implementation of organization testing guidelines in the bundles promotes standardization and compliance.
- Before ordering any tests for infectious diseases, it is crucial to carefully evaluate the pre-test probability of bacteremia and the likelihood of identifying a clinically significant organism. Repeating blood cultures within 48 hours of the initial set typically yields low results. Blood cultures should be collected before initiation of antimicrobial therapy. Indications for blood culture draws may vary depending on the patient population (e.g. adults versus pediatrics, immunocompetent versus neutropenic, inpatients versus from the emergency department) [1, 2]. For certain patient populations, consider performing only two blood cultures (1 set) vs. widely accepted and recommended four blood cultures (2 sets). While this is beyond the scope of this blog post, please refer to the sources below for specific clinical guidance.
- Due to the typically low levels of bacteria present in the bloodstream, collecting a larger volume of blood increases the chances of obtaining a positive culture. To maximize the likelihood of detecting bacteria, blood culture bottles should be filled with the optimal volume recommended by the manufacturer, typically 8-10 mLs up to the fill line, and be sent to the microbiology laboratory in the timely manner. Reducing contamination in blood cultures decreases the need for additional resources, such as repeat blood cultures, unnecessary antibiotic treatments, and further diagnostic tests. Contamination can be minimized by strictly adhering to antiseptic procedures at collection sites, ensuring proper training for collectors. It is also crucial to remind healthcare providers and clinical staff to follow institutional guidelines for proper specimen labeling, maintaining specimen stability, and adhering to transport instructions to reduce the risk of sample rejection and prevent unnecessary waste of supplies [3].
- Thinking outside the box:
- Despite the shortage, patient care continues, and laboratories may need to think of alternative approaches. As of writing this post, other blood culture systems and their respective bottles are not affected. That said, implementing new instruments and switching to an alternative supply chain from a different manufacturer may be an option but often can take up to several months due to contractual requirements. Additionally, massive re-education and training (laboratory staff, phlebotomy, and nursing) will need to take place as different systems have unique collection procedures. Some institutions may opt to send out their blood cultures to reference laboratories that use an alternative system, although turnaround time may be an issue. Manual blood cultures, although laborious, could be set up and be done in-house. While it is not recommended to use expired blood culture bottles, recent published studies have shown that expired bottles up to 3 months are just as effective [4, 5]; institutions should maintain expired bottles if regulatory bodies allow for their utility at an later date as BD have extended the expiration date for certain lots already (see BD manufacturer webpage below). BD has recently announced the re-introduction of anaerobic media in glass bottles. Laboratories should prepare staff and develop plans for validation work to ensure that these bottles can be rapidly implemented for usage.
- Continuous monitoring:
- Aside from monitoring inventory and bottle usage, it is important for laboratories to regularly monitor contamination rates and implement a quality system that tracks blood culture volumes. To allow for targeted and more efficient education, monitoring trends stratified by different departments can help offer specific feedback to the clinical partners collecting the samples.
- As we implement additional testing methodologies, remember to continuously revise your Clinical Practice Guidelines (CPGs), order sets, test utilization, etc. as part of such implementations.
A lesson learned from the COVID-19 pandemic is the need to be agile and quickly adapt to the changes in supply chain. For many laboratories, this was an effective strategy to ensure testing availability for all patient populations. Although this blood culture bottle shortage is a crisis many are facing, implementing diagnostic stewardship for blood culture collection may have overall benefits such as decreasing the amount of unnecessary testing, treatment of clinically insignificant infections, unnecessary blood draws, and potential central line-associated bloodstream infections.
Here are external resources/references available to help laboratories and healthcare providers:
- Manufacturer’s web page: https://bdbactec-update.com/
- American Society for Microbiology (ASM) guideline, endorsed by the Society for Healthcare Epidemiology of America (SHEA): https://asm.org/guideline/blood-culture-shortages-management-diagnostic-stew
- Informational web page from the Infectious Disease Society of America (IDSA): https://www.idsociety.org/clinical-practice/blood-culture-bottle-shortage/
References
1. Fabre, V., K.C. Carroll, and S.E. Cosgrove, Blood Culture Utilization in the Hospital Setting: a Call for Diagnostic Stewardship. J Clin Microbiol, 2022. 60(3): p. e0100521.
2. Fabre, V., et al., Principles of diagnostic stewardship: A practical guide from the Society for Healthcare Epidemiology of America Diagnostic Stewardship Task Force. Infect Control Hosp Epidemiol, 2023. 44(2): p. 178-185.
3. Clinical and Laboratory Standards Institute, Principles and Procedures for Blood Cultures, CLSI guideline M47. 2nd Edition. 2022.
4. Hardy, L., et al., Blood culture bottles remain efficient months after their expiration date: implications for low- and middle-income countries. Clin Microbiol Infect, 2024. 30(10): p. 1327-1328.
5. Klontz, E.H., et al., Evaluation of expired BD BACTEC blood culture vials. J Clin Microbiol, 2024: p. e0108224.

-Rebecca Yee, PhD, D(ABMM), M(ASCP)CM is the Chief of Microbiology, Director of Clinical Microbiology and Molecular Microbiology Laboratory at the George Washington University Hospital. Her interests include bacteriology, antimicrobial resistance, and development of infectious disease diagnostics.

-Olga Kochar, MS, CSSGB, is the Divisional Director of Laboratory and Transfusion Services with the GW Hospital, as well as faculty with the GWU School of Medicine and Health Sciences. With over 29 years in the healthcare industry, Olga Kochar is passionate about quality and patient safety, performance improvement and teaching.
