Case Presentation
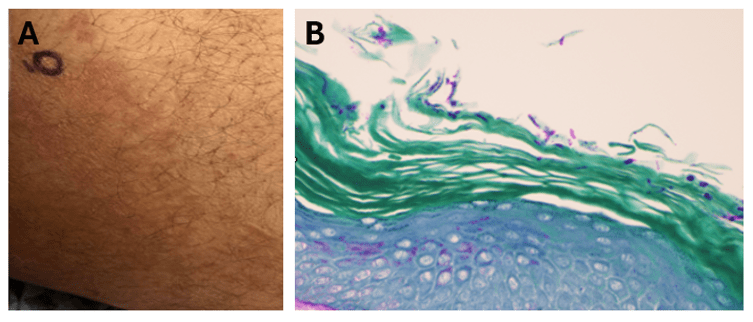
A middle-aged male presented for a chronic inguinal and back rash present for over two years (Figure 1A). Travel history was notable for trips to the Middle East and Canada during that time. He was clinically diagnosed with tinea cruris at an outside healthcare facility, and his history was notable for an extensive use of several topical antifungals including clotrimazole with betamethasone, ketoconazole, and triamcinolone without improvement. Months long oral therapy with terbinafine and fluconazole resulted in only mild improvement, after which he was started on itraconazole. The patient noted some improvement while taking itraconazole, but following subsequent disease recurrence, presented to our institution.
Laboratory workup
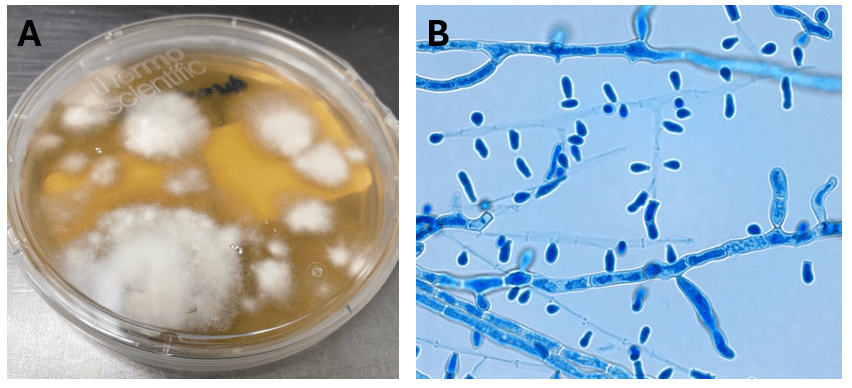
An inguinal skin scraping was obtained, which revealed the presence of a superficial fungal infection consistent with the diagnosis of tina cruris. Fungal cultures on Sabouraud Dextrose Agar (Figure 2A), lactophenol blue stain (Figure 2B), and a skin biopsy (Figure 1B) all confirmed a dermatophyte infection. The organism was morphologically consistent with Trichophyton sp. Due to the unusual clinical history of a recalcitrant dermatophyte infection persisting through multiple rounds of topical and oral antifungal therapy, additional testing for definitive identification was undertaken. MALDI-TOF identified the organism as a member of the Trichophyton tonsurans/mentagrophytes species complex, further confirmed to be Trichophyton indotineae by sequencing.
Discussion
Ringworm, also referred to as “tinea” or “dermatophytosis,” is a commonly occurring fungal infection affecting the skin, hair, or nails, caused by dermatophytes.1 Typical symptoms include itching, a ring-shaped rash, redness, scaliness, cracked skin, and/or hair loss. The transmission of ringworm happens through direct contact between individuals, contact with infected animals, or exposure to contaminated environments such as public showers.1 Around 40 different species of fungi can lead to ringworm infection.2 Over the last decade, healthcare providers have observed a rise in severe cases of ringworm that are resistant to topical antifungal treatment3 which are an emerging public health concern.
The emergence of drug-resistant dermatophyte infections is attributed to the inappropriate use of topical products containing combinations of antifungal agents and corticosteroids.4 T. indotiniae has a complicated taxonomic history. The organism was initially identified as a sequence type of the Trichophyton mentagrophytes complex which exhibited elevated MICs to terbinafine. The earliest cases of T. indotineae infection were reported in India, quickly spreading to Australia, Oman, Iran, and other middle-eastern countries. Subsequent spread to Europe and North America soon followed.5 Initial reports of T. indotineae infections in North America involved individuals with a history of travel to endemic locations. Recently however, local transmission of T. indotineae within the United States has been documented among patients without travel history.6 It is hypothesized that resistant strains of T. indotineae emerged due to inappropriate antibiotic use, as infections are frequently terbinafine-resistant and require prolonged therapies with second-line therapies or antifungals traditionally utilized for invasive fungal infections.7
Diagnosis of T. indotineae infection is challenging as it requires advanced molecular techniques like genomic sequencing or expansion of MALDI-TOF MS capabilities to discriminate within the T. mentagrophytes complex, which many clinical laboratories lack.1 Thus, diagnosis is largely reliant on the activities of reference laboratories. A high level of clinical suspicion is required as well, as the degree of dermatophyte workup undertaken in the routine setting is variable among institutions. T. indotineae infections often show resistance to conventional antifungal therapies including allylamines (terbinafine) and azoles (itraconazole and fluconazole), further highlighting the importance of susceptibility testing before initiating treatment and reassessing nonresponsive cases,4 another testing capability not offered by routine laboratories. The patient in this case was managed with Posaconazole, leading to significant improvements symptomology.
References:
- Emerging antimicrobial-resistant ringworm infections (2023) Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/fungal/diseases/ringworm/dermatophyte-resistance.html (Accessed: 9 April 2024).
- Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwideexternal icon. Mycoses. 2008 Sep;51 Suppl 4:2-15.
- Hay RJ. The Spread of Resistant Tinea and the Ingredients of a Perfect Storm. Dermatology. 2022;238(1):80-81.
- Gupta AK, Venkataraman M, Hall DC, Cooper EA, Summerbell RC. The emergence of Trichophyton indotineae: Implications for clinical practice. Int J Dermatol. 2023 Jul;62(7):857-861. doi: 10.1111/ijd.16362. Epub 2022 Jul 22. PMID: 35867962.
- Jia S, Long X, Hu W, Zhu J, Jiang Y, Ahmed S, de Hoog GS, Liu W, Jiang Y. The epidemic of the multiresistant dermatophyte Trichophyton indotineae has reached China. Front Immunol. 2023 Feb 16;13:1113065. doi: 10.3389/fimmu.2022.1113065. PMID: 36874152; PMCID: PMC9978415.
- Caplan AS, Chaturvedi S, Zhu Y, Todd GC, Yin L, Lopez A, Travis L, Smith DJ, Chiller T, Lockhart SR, Alroy KA, Greendyke WG, Gold JAW. Notes from the Field: First Reported U.S. Cases of Tinea Caused by Trichophyton indotineae – New York City, December 2021-March 2023. MMWR Morb Mortal Wkly Rep. 2023 May 12;72(19):536-537. doi: 10.15585/mmwr.mm7219a4. PMID: 37167192; PMCID: PMC10208369.
- Lockhart, SR, Smith, DJ, and Gold, J.A.W. Trichophyton indotineae and other terbinafine-resistant dermatophytes in North America. J. Clin. Microbiol. 2023 Dec; 61(12): e00903-23. PMID: 38014979.
–Tasnim Alkayyali is a second-year AP/CP resident at UT Southwestern Medical Center in Dallas, Texas.

–Clare McCormick-Baw, MD, PhD, FACP is a board certified Anatomic and Clinical Pathologist with a subspecialty in Medical Microbiology. She has a love for Infectious Disease Pathology and teaching the pathologists of tomorrow. She is the Southwest Regional Medical Director for Quest Diagnostics, Inc and is based out of Dallas, Texas.

–Andrew Clark, PhD, D(ABMM) is an Assistant Professor at UT Southwestern in the Department of Pathology and Director of the Microbiology Laboratory at Parkland Health and Hospital System. He completed a CPEP-accredited postdoctoral fellowship in Medical and Public Health Microbiology at National Institutes of Health.
