Case History
A 59-year-old man presented to the Emergency Room with bright red blood per rectum, associated with nausea, vomiting, abdominal cramping, and persistent watery diarrhea. Several days earlier, he had returned from a three-week trip to the Dominican Republic. On physical examination, he was afebrile. His abdomen was soft and not tender or distended.
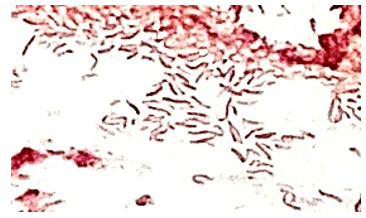
A stool sample was sent to the Microbiology Lab for PCR testing, and both Vibrio and Vibrio cholera targets were detected. The stool was then plated for culture confirmation. Hemolytic colonies grew on the blood agar plate (Figure 1), and yellow (original medium color green) colonies grew on thiosulfate citrate bile sucrose selective agar due to sucrose fermentation (Figure 2). Gram stain from these colonies showed gram negative, curved, comma-shaped rods (Figure 3) and MALDI-ToF identification revealed Vibrio albensis. The specimen was sent to the Department of Public Health for confirmation, which reported Vibrio cholerae O1 serovar Ogawa with O1 antigen typing.


Discussion
Vibrio albensis is a gram negative, halophilic bacterium belonging to the Vibrionaceae family. V. albensis is a recently identified species within the Vibrio genus and is believed to be a member of the Vibrio cholera complex. Although primarily considered non-pathogenic, V. albensis has been associated with rare cases of human infections, particularly in individuals with compromised immune systems.1 While previously reported studies indicated V. albensis as a non-O1, non-O130 serogroup of V. cholerae,2the Department of Public Health confirmed our patient’s isolate as O1 serovar Ogawa by O1 antigen typing. V. albensis is an emerging pathogen with limited information regarding its clinical significance and optimal management. The infections are predominantly associated with contaminated seawater or seafood exposure. The primary transmission mode is through open wounds or ingesting raw or undercooked seafood.3
Clinical presentation of this organism can be similar to V. cholerae, as diffuse watery diarrhea, the hallmark of cholera, or asymptomatic. Other case reports presented bacteremia, septicemia, and urinary tract infections.4,5
Laboratory diagnosis of Vibrio cholerae albensis infection involves isolating and identifying the bacterium from stool samples. This can be achieved using selective culture media, such as thiosulfate-citrate-bile salts-sucrose (TCBS) agar, which allows for the growth of V. cholerae and its variants.6
Antimicrobial resistance is a growing concern in the management of cholera. Studies have reported varying resistance levels to commonly used antibiotics in V. cholerae, including V. cholerae albensis. It is essential to monitor antimicrobial susceptibility patterns to guide appropriate treatment strategies.7 Further research is needed to better understand the epidemiology, clinical manifestations, and optimal treatment strategies for V. albensis infections as members of V. cholerae complex are being identified/recognized with more advanced diagnostic tools.
References
- Baker-Austin C, et al. (2016). Vibrio albensis sp isolated from a mesophilic bacterial culture, abalone (Haliotis spp.), and seawater. International Journal of Systematic and Evolutionary Microbiology, 66(1), 187-192.
- Ahmed AOE, Ali GA, Hassen SS, Goravey W. Vibrio albensis bacteremia: A case report and systematic review. IDCases. 2022 Jun 30;29:e01551. doi: 10.1016/j.idcr.2022.e01551. PMID: 35845827; PMCID: PMC9283503.
3. Sharma P, et al. (2018). Vibrio albensis: An Emerging Pathogen Causing Necrotizing Fasciitis. Journal of Clinical Microbiology, 56(3), e01454-17.
4. Araj GF, Taleb R, El Beayni NK, Goksu E. Vibrio albensis: An unusual urinary tract infection in a healthy male. J Infect Public Health. 2019 Sep-Oct;12(5):712-713. doi: 10.1016/j.jiph.2019.03.018. Epub 2019 Apr 10. PMID: 30981654.
5. Sack RB, et al. (2004). Cholera. The Lancet, 363(9404), 223–233.
6. Centers for Disease Control and Prevention (CDC). (2021). Laboratory Methods for the Diagnosis of Vibrio cholerae. Retrieved from https://www.cdc.gov/cholera/laboratory.html
7. Ceccarelli, M., et al. “Editorial–Differences and similarities between Severe Acute Respiratory Syndrome (SARS)-CoronaVirus (CoV) and SARS-CoV-2. Would a rose by another name smell as sweet.” European review for medical and pharmacological sciences 24.5 (2020): 2781-2783.

-Eros Qama, MD, is a 2nd year AP/CP pathology resident in the Department of Pathology at Montefiore Medical Center in Bronx, NY

-Phyu Thwe, Ph.D, D(ABMM), MLS(ASCP)CM is Associate Director of Infectious Disease Testing Laboratory at Montefiore Medical Center, Bronx, NY. She completed her medical and public health microbiology fellowship in University of Texas Medical Branch (UTMB), Galveston, TX. Her interests includes appropriate test utilization, diagnostic stewardship, development of molecular infectious disease testing, and extrapulmonary tuberculosis.
