A 35 year old male and current every day smoker transferred his care to our genitourinary (GU) clinic after undergoing a partial nephrectomy for clear cell renal cell carcinoma. A PET scan was performed, and a 5 millimeter FDG-avid right upper lobe (RUL) lung nodule was identified. While the mediastinal and hilar lymph nodes were mildly enlarged on the chest CT, they did not demonstrate FDG-avidity on the PET scan. The patient was referred to pulmonary for a workup of his subcentimeter lung nodule. Given the patient’s age and clinical history, the care team and the patient decided to pursue a lung biopsy via robotic-assisted bronchoscopy and subsequent lymph node sampling via endobronchial ultrasound (EBUS).
After the timeout, the patient was intubated, and the pulmonologist performed an airway inspection. Upon entering the right upper lobe, the pulmonologist noticed blood streaking along the bronchial wall. A right upper lobe bronchoalveolar lavage (BAL) was collected and sent for culture and cytology. Following the trachea and lung survey, the respiratory team began the robotic-assisted bronchoscopy. After confirming the correct location with both radial EBUS and fluoroscopy, multiple fine needle aspirates (FNAs) were collected from the right upper lobe lung nodule. Only benign bronchial cells were identified on rapid onsite evaluation (ROSE). A right upper lobe bronchial brushing was attempted and sent directly to cytology. Forceps were used to obtain transbronchial biopsies from the radiologically-suspicious area. The team then switched over to linear EBUS for the lymph node sampling portion of the procedure. Lymph nodes were sampled at the following stations: 11L, Level 7, and 4R. On ROSE, only lymphocytes and anthracotic pigment were identified for all three lymph nodes.
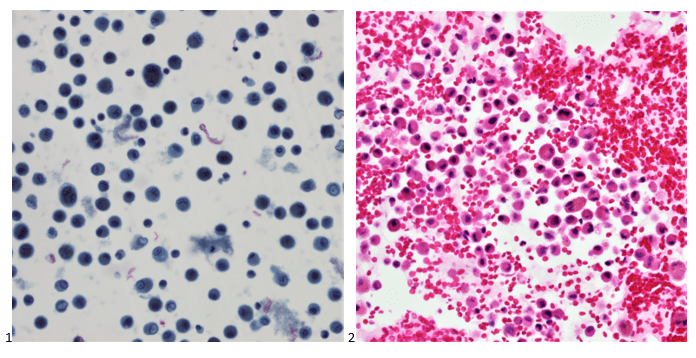
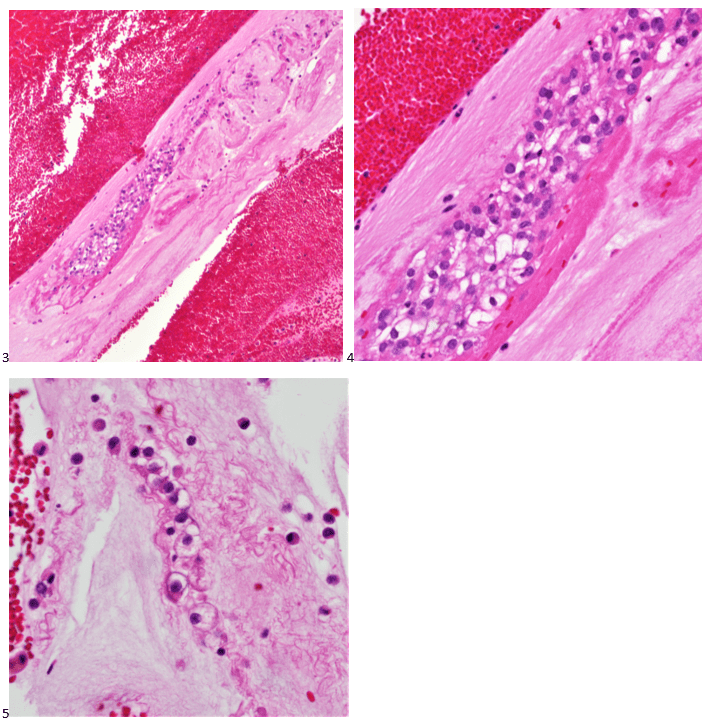
Upon e, the cytologist brought the specimens back to the laboratory for accessioning and processing. The following morning, the same cytologist screened all cytology specimens and the respective cell blocks associated with the case. The lymph nodes were signed out as negative for malignancy, with lymphocytes and anthracotic pigment present. The RUL FNA was inadequate for diagnosis as the material consisted mainly of bronchial cells and alveolar macrophages. The FNA findings were correlated with the transbronchial biopsy, which was signed out as benign pulmonary parenchyma with hemorrhage, fibrin clot, and respiratory bronchiolitis. Similarly, the bronchial brushing was negative as only benign bronchial cells were identified. In screening the BAL, there was an overabundance of hemosiderin-laden alveolar macrophages on the smear, cytospin, and SurePath liquid-based preparations (Image 1). When screening the cell block slides, abundant macrophages were also identified (Image 2).
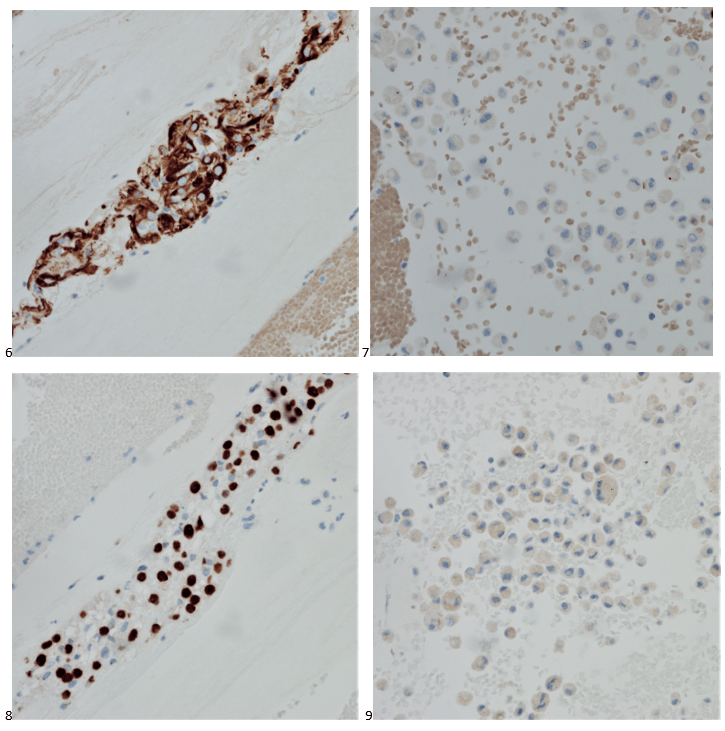
However, in the cell block sections, the cytologist also identified cells stranded within areas of mucin (Image 3). It may have been easy to dismiss these as macrophages, but contrary to the dusty hemosiderin-laden macrophages in this specimen, these cells had abundant vacuoles, and irregular nuclei with more prominent nucleoli (Images 4-5). The pleomorphic nuclei and larger vacuoles distinguished these cells from lipid-laden macrophages most often seen in aspiration pneumonia.
The cytologist, marking the areas of interest, swiftly rendered a diagnosis of positive for malignant cells, favoring metastatic clear cell renal cell carcinoma. She enthusiastically described the case to the attending cytopathologist, who immediately ordered confirmatory immunostains on the unstained paraffin sections of the cell block.
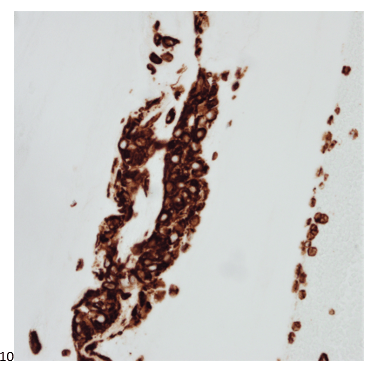
With adequate controls, CD68 highlights the alveolar macrophages (not shown). The tumor cells show positive staining for AE1/AE3 and PAX-8 (Images 6-7), while macrophages show negative staining for AE1/AE3 and PAX-8 (Images 8-9). The tumor cells also show positive staining for vimentin (Image 10) and RCC (focal), and negative staining for TTF-1.
RUL BAL Final Diagnosis: Positive for malignant cells. Metastatic clear cell renal cell carcinoma.
When we attend a biopsy of an area clinically suspicious for metastatic renal cell carcinoma, we prepare ourselves for an overtly bloody sample. Even if the smears consist mainly of blood during ROSE, we rest assured that we will usually find tumor cells in the cell block sections. By obtaining a BAL of the blood-streaked RUL, the pulmonologist was able to pinpoint an area of lymphangitic spread. We often give little credit to BALs in cytology, especially when using concurrent techniques such as FNAs to sample a subcentimeter lung nodule without bulky disease. However, as seen in this case, sometimes it’s the only specimen that can help us render a diagnosis of metastatic cancer.

-Taryn Waraksa-Deutsch, MS, SCT(ASCP)CM, CT(IAC), has worked as a cytotechnologist at Fox Chase Cancer Center, in Philadelphia, Pennsylvania, since earning her master’s degree from Thomas Jefferson University in 2014. She is an ASCP board-certified Specialist in Cytotechnology with an additional certification by the International Academy of Cytology (IAC). She is also a 2020 ASCP 40 Under Forty Honoree.
